Mosquito-borne diseases are not usually a hot news topic in North America, despite the fact that nearly half a million lives were lost to malaria just last year. Recently, however, Zika fever, a member of the group known as “neglected tropical diseases”, has been dominating the media. The Zika virus is primarily transmitted by the females of the Aedes aegypti (and Aedes albopictus) mosquitoes. The disease crept into Brazil last summer, taking most by surprise.
I was in Brazil in 2013 discussing with Brazilian researchers the application of fast diagnostic methods for dengue fever (the most common member of the Zika family, dengue is a disease that affects about 400 million people every year worldwide), and they were very concerned with the appearance of the first cases of Chikungunya (another of Zika’s cousin) in Brazil. There was no mention of Zika. It was simply not on their radar.
Zika fever (first discovered in 1947) was virtually unknown (only about 14 cases were formally documented before 2007) and mainly confined to tropical Africa, Southeast Asia, and the Pacific Islands. The Brazilian Zika outbreak in 2015 raised concerns, but appeared to be a relatively mild problem when compared to both dengue and Chikungunya. Although all three diseases (Zika, dengue and Chikungunya) share the same vector and present similar symptoms (fever, skin rash, headache), the effects (mainly muscles and joint pain) are generally less debilitating in Zika than for the others. Moreover, Chikungunya and dengue appeared more prone to further complications than Zika.
Overall, Zika seemed to be the less threatening of the Aedes-transmitted virus family. However, a few months after the first Zika outbreak, Brazilian health officials started to observe a much higher than normal incidence of microcephaly and other severe birth defects from regions that had been hardest hit by Zika. Babies with microcephaly have much smaller heads, due to improper development of the brain during pregnancy. The condition can lead to several problems, including very slow cognitive development; seizures; difficulties in dealing with routine voluntary movements, such as swallowing; hearing and vision impairment. A direct causal relationship between Zika and those birth defects was confirmed last April. A relationship between Zika and other complications such as Guillain-Barré syndrome has also been established.
These discoveries have triggered alarm bells across the world. Zika virus was declared a “public health emergency” by the World Health Organization (WHO) in February 2016 for two reasons. First, Zika is spreading at a breathtaking velocity. Zika outbreaks are not only confined to Brazil and have reached most of the Latin America and Caribbean regions. Active Zika virus transmission (through mosquito bite) has reached as far as the North states of Mexico. Although no locally-acquired Zika case has been reported in the continental USA, almost 2,500 people were infected by mosquito bites in Puerto Rico. The ferocity in which Zika moved North from Brazil suggests that some southern states in the continental USA could fall victim of the disease soon. In contrast to dengue and Chikungunya, Zika virus has been isolated in semen and cases of sexual transmission have been confirmed. There is also some evidence that Zika can be transmitted through deep kissing, since the virus has been found in saliva.
Most of the established Zika cases in Canada (~150) are travel associated, which leads to the second reason for Zika’s world-wide prominence. In August 2016, Rio de Janeiro will host the Olympic games, arguably the most popular sports event in the World. Therefore, Brazil will receive millions of tourists and thousands of athletes. Although the incidence of Zika from the 2016 outbreak in Brazil is declining (the games will be in the winter in the southern hemisphere, therefore, the mosquito population will have diminished significantly) and the risk of infection is lower, the situation cannot be taken lightly; mainly for women who are or intend to be expecting in the near future.
Canadians who are planning on attending the games (or, more generally, who are planning to travel to Zika affected areas) must take some important precautions. The use of mosquito repellent and the wearing of long sleeves and long paints are simple common sense provisions. Pregnant women should take extra care and immediately see a doctor if they experience any flu-like symptoms.
The fact that Zika is potentially transmitted sexually greatly raises concern. Zika symptoms are sometimes mild and an infected man might not even realize that he is sick. This means that men can unknowingly pass the virus to his partner. In fact, the virus appears in the semen even before the development of symptoms of the disease, and then it remains after the symptoms have ceded. The Zika virus persists in semen longer than in blood, but it is unknown for how long. All this means that the use of condoms (or sexual abstinence) is highly recommended for travellers. Since the lifetime of the Zika virus in semen is unknown, it is better to be on the safe side and continue to use condoms for six to eight months after returning from travel to a Zika affected area. It is also a good idea to postpone any plans to conceive for at least six months.
There is no specific treatment for Zika virus infection. The disease is managed like the common flu; with acetaminophen or paracetamol to control fever (aspirin and non-steroidal anti-inflammatory drugs (NSAIDS) are not recommended), plenty of rest and fluids to avoid dehydration. Antihistamines can be used to help with the itching. Experimental Zika vaccines have been approved for first human trials (including one vaccine developed by a collaboration between researchers from the Université Laval in Quebec and US partners), but there is nothing available yet.
The bottom line is that the response to Zika outbreaks has focused on the time tested solution used for all mosquito-borne diseases around the world – to kill the mosquito. It turns out that decimating a mosquito population is not as straightforward as it sounds. Simple techniques, such as mosquito traps, can be useful. Avant-garde methods include the use of genetically modified mosquitos or the introduction of a large population of radio-sterilized males that are able to mate but leads to inviable female eggs. Currently, the most efficient approach for mass-destruction of mosquitoes is the use of insecticides and larvicides. However, it is not practical to “spray” indiscriminately large densely populated areas in urban settings.
A good amount of logistics is involved in deciding where and how to deploy measurements for mosquito control. Governmental health organizations in affected countries generally employ an army of public health officers (PHOs). In Brazil, PHOs go door-to-door around neighborhoods to check standing water in items such as tires, flower pots and toys for the presence of the larvae and the mosquito. They arrive armed with official brochures and posters in an attempt to educate the general public on simple methods to control potential mosquito breeding grounds. They then report the infested areas back to the government. These reports then guide the spraying.
It is clear that this process (which has been repeated every year for decades) is inefficient and time-consuming. The significant delay between the report and response allows the disease to spread. Better surveillance technologies are required to improve response time and containment of the outbreaks.
Over the last 15 years, my research group has been exploring optical effects (colors) observed in very small gold chunks (“nanogold” – gold pieces that are 1000’s times smaller than the diameter of a human hair). As the Zika crisis developed, we decided to use this expertise in nanotechnology to provide the PHOs with a new tool that would allow them to report the presence of Zika in real-time.
The idea is to develop a low cost platform that consists of immobilizing “nanogold” in a simple plastic strip and then coat it with a Zika virus antigen. The result is a biosensor that looks like a litmus test for Zika. The plastic strip changes color when in contact with Zika infected saliva. We decided to target saliva, rather than blood (which is more common for Zika diagnosis), for two reasons: 1) the goal is to provide a tool for PHOs. They generally do not have medical training and are not equipped to handle complex biological samples; 2) the amount of Zika virus is actually high in saliva. Saliva sampling is also easier to extract from infants, children and the elderly. The material cost per strip is less than CDN $5.00. If mass-produced, the cost per strip could be less than $1.00.
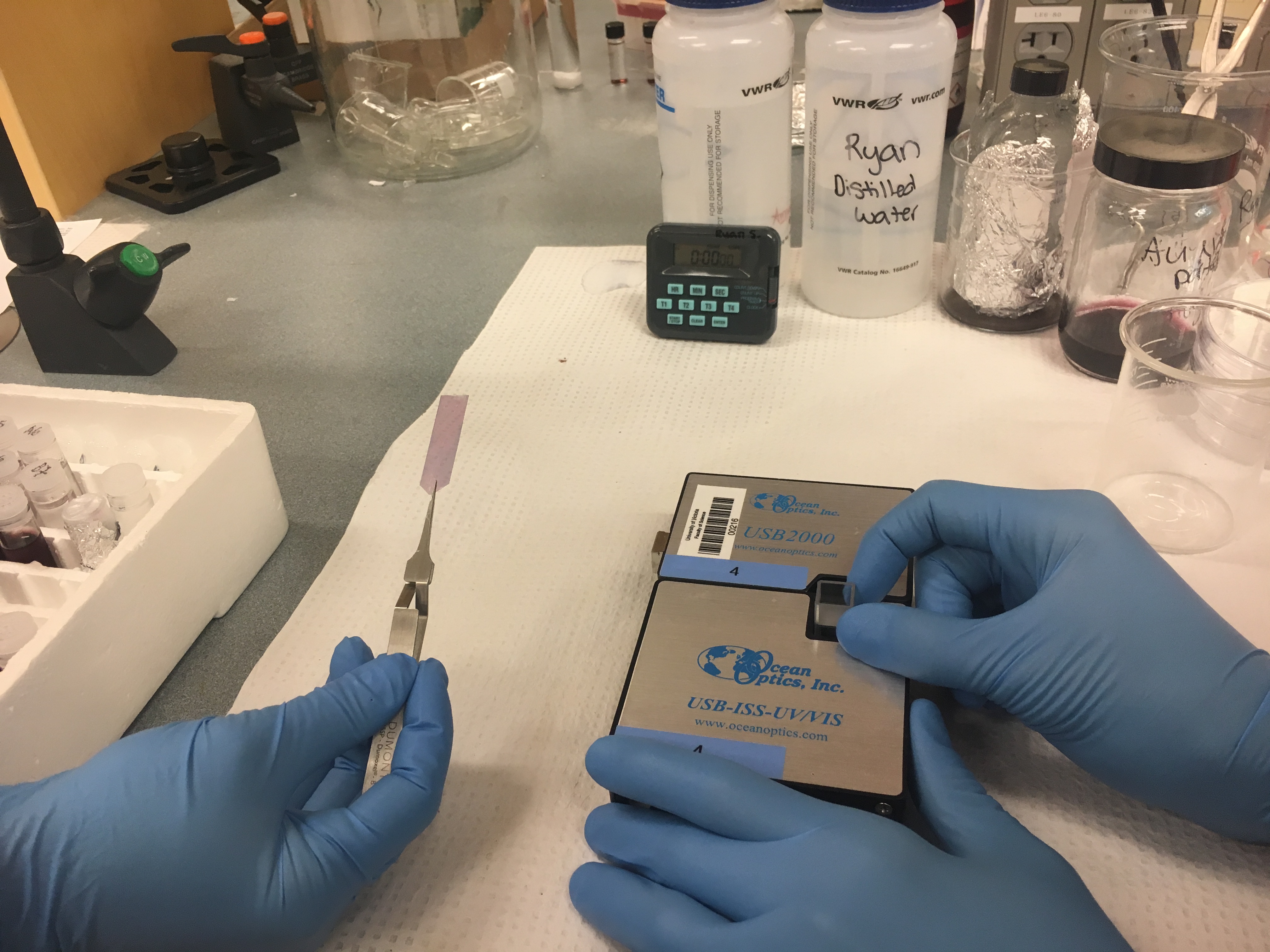
The vision is to equip PHOs with the strips and a piece of hardware (“reader”) attached to their cell phones. The hardware will quickly detect the presence of Zika (by measuring the color change), and upload the location of the contaminated individual in real-time (in Google maps, for instance). This would allow health officials to monitor trends and the spread of the infection instantly, leading to a more rapid response and deployment of resources.
The initial steps to develop this technology have recently been funded by a Zika Innovation Award from Grand Challenges Canada (https://www.grandchallenges.ca/). This seed grant has led to successful preliminary proof-of-concept experiments realized here in Victoria (saliva from health students spiked with Zika antibodies were used in the experiments). We are now in the process of ramping up production of the plastic strips to deploy them in a pilot test in Brazil next August. Another goal in the near future is to develop specific strips also for dengue and Chikungunya, so a PHO would be able to report not only the presence of the infection, but also the type of disease in a particular area. The technology is still in the early stages of development and we are still fighting non-specific detection (false positives).
Considering the potential individual impact of Zika, it is possible that our technology might one day be used as an off-the-shelf test, available in regular clinics and drug stores. The low-cost plastic strip test could then be a new tool for prenatal care in countries infested with Aedes mosquitoes.
Beyond the obvious health concerns, Zika carries other global consequences. For instance, the governments of Colombia, El Salvador, Jamaica and (of some States in) Brazil advised women to postpone their plans to have a child. It is estimated that Brazil alone had around 350,000 less births in 2015-2016 due to Zika concerns. This means that some kindergarten classrooms in those Countries will be between 10 – 30 per cent emptier only six years from now due to this crisis. It is also important to point out that birth control strategies in several of the Latin American and Caribbean Countries are not accessible to the majority of low-income families, and they are the ones who will have to deal with the devastating effects of the disease in newborns. This points to a bleak future unless advance technologies for mosquito control, disease surveillance, prevention and diagnosis are generated. It is our hope that our low cost screening method will play an important role in managing this global crisis.
Zika Facts and Figures
- Zika has been reported in 40 countries and two US territories in the Americas.
- It is estimated that only about 1 in 4 people infected with Zika virus develop noticeable symptoms.
- It usually takes between 3 to 12 days for symptoms to appear after infection. The disease symptoms are usually mild and last for 2 to 7 days.
- About 430,000 of suspected Zika cases have been reported in the Americas between 2015-2016.
- Only 9 deaths have been directly linked to Zika (excluding the ones related to microcephaly and other Zika consequences) in the Americas between 2015-2016.
- About 3,000 newborns with microcephaly were reported in Brazil in 2015.
- The average incidence of Zika in Brazil in 2016 is about 80 cases per 100,000 habitants. However, the 2016 average incidence in the state of Rio de Janeiro (Olympic venue) is about 280 cases per 100,000 habitants. The estimate incidence during the games (winter) should be less than 5 cases per 100,000 habitants.
- There were 162 cases of Zika in Canada. 161 were travel-related and 1 was sexually transmitted. No Zika related deaths or birth defects have been reported in Canada.


