GPS for early lung cancer detection could increase five-year survival rate
By Melicent Lavers-Sailly
Early detection for lung cancer is an ongoing challenge. Like most cancers, lung cancer survival rates are directly tied to the stage at which it is found. According to the Canadian Cancer Society, early-stage lung cancer patients have a 50 per cent five-year survival rate. However, as stages advance, that may drop to single digits. Unfortunately, nearly half of lung cancer cases are diagnosed at an advanced stage. Based on 2016 data, the lung cancer five-year net survival is approximately 14 per cent for males and 20 per cent for females.
There are a number of reasons why early stage detection is such a challenge; the first being that patients often mistake symptoms such as coughing, shortness of breath, fatigue and hoarseness with other conditions. As such, they don’t seek medical attention until they have worsened, at which point the cancer may already be at Stage 3 or 4. In other cases, lung cancer is found by accident when the patient is being investigated for something else.
The nature of the disease itself is another factor. Lung cancer tends to begin in the periphery of the lungs, an extremely difficult area to reach in order to conduct an accurate biopsy.
Another challenge is the screening procedures. There has been no definitive screening test that is generally available to all patients; and the conventional test procedures used can be invasive, inaccurate, and present higher risks to patients. However, there is now GPS-based technology that is resolving many of those challenges and bringing new hope to lung cancer patients.
Let us first consider the conventional options. Procedures such as TTNA (transthoracic needle aspiration), a needle biopsy conducted through the thorax, carries a 42 per cent risk of pneumothorax (lung collapse); a 17 per cent risk of requiring a chest tube insertion; and a 10 per cent risk of hemoptysis (spitting up of blood) and hemorrhaging.
A thoracotomy (surgical removal of lung tissue) brings with it a higher risk of morbidity and mortality and cannot be used on compromised patients. In addition, many of these surgeries prove to be unnecessary as many lesions are benign (20 to 45 per cent).
Periodic CT scanning, while not as invasive, is often used in cases where a highly compromised patient may not be able to tolerate TTNA or surgery. Understandably, there is a higher degree of probability that the cancer will grow.
With traditional bronchoscopy — the process of inserting a lighted tube through the nose or mouth to evaluate lungs and collect tissue samples — it is especially challenging to reach deep into the lungs where most lesions are found. The failure rate stands at 65 per cent, which often means additional invasive procedures are needed.
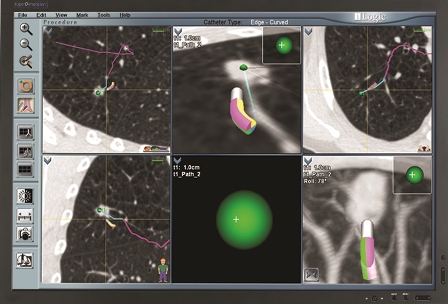
Yet there is another option for early detection of peripheral lung cancer that reduces the need to conduct more invasive procedures, while resolving the accuracy challenges in bronchoscopy. Known as ENB (electromagnetic navigation bronchoscopy), the technology uses GPS-based technology to accurately and safely navigate a bronchoscope into difficult to reach areas of the lung.
ENB technologies, such as Medtronic superDimension™ Navigation System, offer an opportunity to aid in earlier diagnosis, with low complication rates, and high diagnostic yield.
In simple terms, a CT scan image is imported into the LungGPS™ Technology to create a 3D bronchial map that connects the trachea to the intended targets in the safest and most efficient way possible. During navigation, the map is matched to the patient’s anatomy to provide interactive pathway guidance to the target.
ENB can play a key role in helping physicians diagnosing earlier, with far less complexity and risk. Lung tissue collection is also optimized to deliver more accurate results, which translates into faster, more effective treatment. The technology also helps doctors from having to engage in multiple procedures to gain the same outcomes. Considering these advantages, the benefits for the patient and the healthcare system are clear.
Melicent Lavers-Sailly is the PR & Corporate Communications Manager, Medtronic Canada.