The November 2013 “Pain in Canada fact sheet” published by the Canadian Pain Society states some hard facts summarized under the heading Pain is Poorly Managed in Canada. These facts include:
- Canadians are left in pain after surgery even in our top hospitals
- Surgery itself if the cause of almost 10 per cent of chronic pain in Canada
- Pain is the most common reason for seeking healthcare (78 per cent of ER visits)
- One in five Canadian adults suffer from chronic pain
- One in five Canadian children have weekly or more frequent chronic pain
- Chronic pain is associated with the worst quality of life as compared with other chronic diseases
- The annual cost of chronic pain in Canada is $56-60 billion dollars
If we are [officially] practising “Evidence-Based Medicine” in Canada, why is the “empirical evidence” presented above showing that we are seriously failing to treat pain? One answer, based on the hard data that shows where money is spent in the medical systems of developed countries, is that… even though “pain is a puzzle” with many pieces, we are approaching its treatment in an oversimplified manner, favoring pharmacological and surgical interventions over any other approach.
MORE: ACUPUNCTURE FOR PAIN? NO THANKS
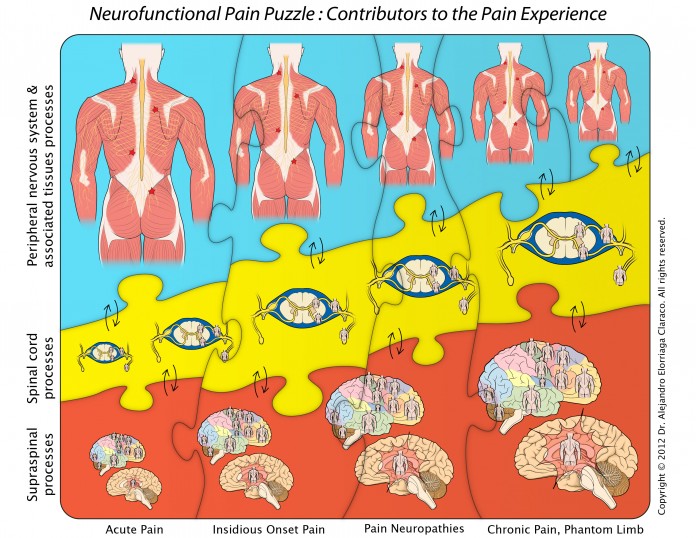
For many years, scientific knowledge of pain has been providing new clues to help us understand “the pain puzzle.” Perhaps the most important scientific fact regarding pain is that the experience of pain is paradoxical: while pain is perceived “as if” occurring in the body, in actuality, pain is the result of the brain’s integration of complex neurological activity involving cognitive, affective and sensory dimensions, what Dr. Melzack termed years ago “the neuromatrix.” The immediate corollary is that if “pain is in the brain” it should be there where we need to start solving the pain puzzle.
In addition to the brain dimensions, there are other contributors to the “pain puzzle” also identified by science, such as the peripheral nerve pathways involved in the transmission and processing of “unpleasant sensory information”, as well as the many spinal cord processes that influence the final passage of these signals to the brain.
As a reflection of its phenomenal complexity, the physiology of the pain experience involves all our important levels of function: neurological, metabolic, hormonal, immune, visceral, biomechanical and psycho-emotional.
MORE: ACUPUNCTURE TURNS ADDICT INTO BELIEVER
With this picture, it’s not surprising that chronic pain research has proven the most effective approach to the management of pain is the bio-psycho-social model. This model proposes that health is best understood in terms of a combination of biological, psychological, and social factors rather than purely in biological terms.
Why then are we are still treating pain in daily practice armed mainly with pills, injections and surgical scalps? Well, that is a $60 billion dollar question for Canadians ($600 billion for the USA). The answer? Self evident: consumers of healthcare are extremely naïve expecting that a system dominated by multibillion dollars interests (pharmaceuticals, diagnostics, etc.) would care to change a working model that produces phenomenal profits year after year. Really?
Well, ponder this undeniable fact, based on hard cold data from the Organisation for Economic Co-operation and Development: pharmaceutical expenditure and diagnostics are bankrupting the medical systems of developed countries without providing any additional value to our health.
MORE: SPINE STIMULATION TINGLES THE PAIN AWAY
What could then be the solution to the pain puzzle? Evident too, all true solutions start with ourselves. If we want the Canadian medical system to provide a true science based approach to the treatment of pain, we have to start by giving ourselves a better education in this and other health related topics (becoming responsible consumers), so we can then question the clinical models that are failing to provide pain relief to so many of us. Otherwise, like in physics, things will just keep moving in the direction where forces push them.
For practitioners, we now know enough to start using a more refined diagnostic and treatment model that favors interventions that modulate neurofunction at all relevant levels. Interventions such as electroacupuncture and manual techniques, complemented then with appropriate interventions, including pharmaceutical agents when they have a well-defined role to play. If evidence-based medicine tells us that only a minority of chronic pain is associated with inflammation, why are anti-inflammatories one of the most prescribed drugs to chronic pain patients?
Perhaps we can find an explanation from the same “Pain in Canada fact sheet” mentioned before: Veterinarians receive five times more training in pain management than people doctors.