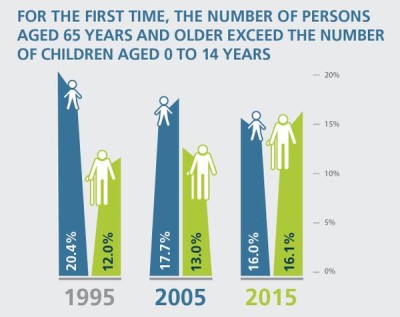
There’s no doubt about it, Canada’s population is aging. Last September, Statistics Canada reported that for the first time in our country’s history, seniors now outnumber children. All of us can expect to live longer. This is a good thing, but it does raise an important question: how do we want to live out our elderly years?
None of us wants to fall ill, become dependent on others or be in and out of the hospital. We all think we’ll stay healthy and independent for as long as we can.
But aging does have its challenges. Growing older means adjusting to a new phase of life. Perhaps you’re leaving the workforce and entering retirement or you’re adjusting to a life without a long-time spouse or partner. Our bodies start to slow down and we may have more trouble getting around and doing the activities we’re used to, such as walking to the nearest shopping centre. We’re also more likely to suffer from multiple chronic conditions as we age.
So how can we ensure that people in their 60s, 70s, 80s, and beyond are given the support they need to remain robust, active and functional members of our society?
Unfortunately, in Canada we have a patchwork of services and resources that vary from one province to another. Access to high-quality care in the community is limited, hospitals are jammed—often with senior patients waiting for placement in a nursing home— and wait times for tests and procedures are growing by the day.
These inefficiencies in our health care system have major financial implications as well. #The Canadian Medical Association estimates that the warehousing of seniors in hospital beds—seniors who could be getting more appropriate care in a home or long-term care facility — is costing the system an extra $2.3 billion a year unnecessarily.
If that’s not shocking enough, perhaps you’d be interested to know that caring for a patient in a hospital bed costs the system approximately $1,000 a day, whereas a long-term care bed costs $130 and home care, $55.
In Ontario specifically, seniors represent about 15 per cent of the population but account for almost half of the province’s health care costs. Ontario’s not alone in this—other regions with “older” populations—Atlantic Canada, Quebec, and British Columbia—are struggling to meet the health care needs of their populations as well.
As a family physician from Nova Scotia, the province with the highest number of seniors per capita, patients share their fears and concerns with me every day. I can tell you some of the realities that my patients face, both seniors and the unpaid, family caregivers who care for them.
Some are not filling prescriptions or they’re skipping medication due to cost, others can’t afford to pay for home or long-term care and many face long wait times for their next test or procedure. The other half are feeling stressed, overburdened and ill-equipped to provide full-time care for their aging loved one.
This is unacceptable; patients need and deserve better.
Part of the reason for these challenges is that our health care system was built over half a century ago to meet the needs of a much younger population. Hospitals were never made to be in the housing business, but this is the new reality we have come to accept.
 The good news: we can change this, while also saving our system money and providing patients with better care. In order to make sure our seniors are getting the care they need, when and where they need it, our country needs a coordinated approach. We need to start talking about spending smarter—by putting money towards palliative care services and long-term care facilities in the community, for example.
The good news: we can change this, while also saving our system money and providing patients with better care. In order to make sure our seniors are getting the care they need, when and where they need it, our country needs a coordinated approach. We need to start talking about spending smarter—by putting money towards palliative care services and long-term care facilities in the community, for example.
We need a national strategy, a national seniors strategy.
This strategy would focus on providing patient-centred care outside of the hospital—care that would be more appropriate and cost less, ultimately benefiting the system as a whole.
The CMA took action on this issue. Over the past year, we’ve engaged with over 70 organizations and the public to draw attention to seniors care. We’ve partnered with members, stakeholders and the public to “Demand a Plan” for a #national seniors strategy.
After gaining over 30,000 supporters in less than a year, the Demand a Plan campaign has shown how strongly Canadians feel about the urgent need to improve the way we care for our seniors.
Supporters have sent over 40,000 letters to Parliamentarians demanding better healthcare for seniors across the country. They’ve also shared messages of support over 16, 000 times on Facebook, Twitter and Instagram, spreading the word on the need for change.
These efforts have not gone unnoticed, as we now have a federal government pledging to ensure our health care system adapts to the needs of our aging population. Specifically, the government plans to invest in a long-term funding agreement with the provinces and territories. This includes increased collaboration and innovation across the country.
However, this is not action for governments alone. Yes, we are looking to the government for leadership and oversight on this, but a meaningful seniors strategy must have the input and support of a broad coalition of stakeholders.
Providers and policymakers must work together to implement programs like palliative care in the home, as well as telehomecare, including home monitoring for therapies, exercise programs, vital statistics, critical responses and crisis support.
In the town of Deep River in the Ottawa Valley, the staff at North Renfrew Long-Term Care Services have figured out a system of care that saves money and provides better care to all patients in the community.
Their services include long-term care beds, supportive care apartments, 24-hour in-home support, respite care, day programs, meals-on-wheels and transportation.
On top of this, the facility has a partnership program with the Renfrew County paramedics who work alongside the personal support workers for two days a week, eight hours a day, visiting clients’ homes and fulfilling their medical needs. This prevents seniors from making frequent and sometimes unnecessary visits to the hospital.
It’s a perfect micro-model of home care for everybody that doesn’t sacrifice quality for efficiency.
If we want our health care system to be able to meet the needs of our aging population, we need to move from the micro to the big picture. That means bringing care to the people who need it, not the other way around.
In other words, we need to understand and be empathetic to the realities faced by patients and their families. Let’s build on this momentum and take this unique opportunity to think about how we can do things better.



Comments are closed.