CJ, a 50-year-old female, walks into the pharmacy, excited to learn that pharmacists can now prescribe for minor ailments, such as gastroesophageal reflux disease (GERD). She asks for a renewal of Pantoprazole (a proton pump inhibitor or PPI) for her GERD, mentioning that she has been taking it daily for years and is afraid to stop.
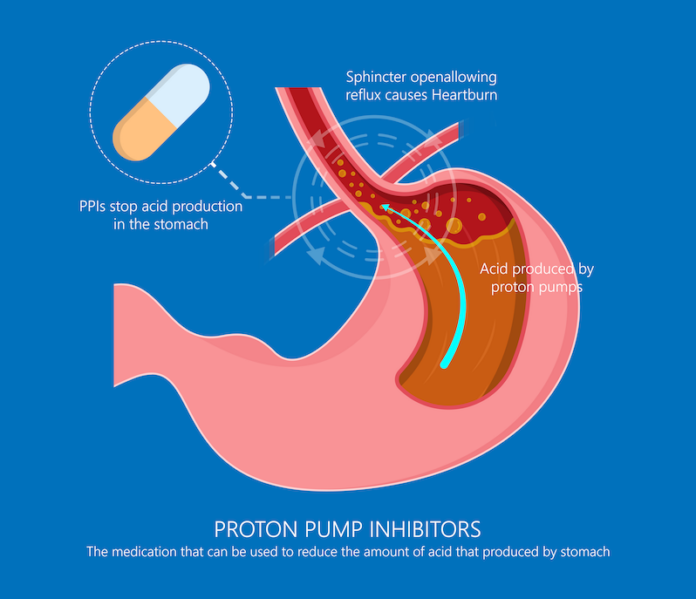
Proton pump inhibitors (PPIs) are one of the most commonly used medications in a variety of healthcare settings (e.g., ambulatory care, hospitals, or community care, etc.). They are often indicated for gastrointestinal disorders, such as, acid reflux, Helicobacter pylori (H. pylori) infections, esophagitis, GERD, and/or peptic ulcer disease. PPIs work by suppressing stomach acid secretion to help relieve heartburn and acid reflux.
The American Gastroenterological Association’s Best Practice Advice Statements recommend deprescribing considerations when there is no clear indications for PPIs use.
PPIs might be taken longer than necessary, most often unintentionally. Although PPIs are very useful for various indications, they can also cause a variety of adverse effects with prolonged use. Oftentimes patients are prescribed a PPI during their hospital stay; and upon discharge, they may continue to take it without a pre-determined stop date. Some of the long-term side effects of PPIs include kidney and heart related disorders, osteoporosis related fractures, infections, and micronutrient deficiencies, etc.
Short-term use of PPIs
There are several reasons why patients are prescribed short-term PPIs. For instance, PPIs are commonly prescribed for one to two weeks alongside antibiotics to treat H. pylori infections. Additionally, a course of four to 12 weeks may be recommended for individuals with stomach or small intestine ulcers, or for esophageal
inflammation.
Long-term use of PPIs
Some patients with specific conditions may need to take PPIs long-term, however it is important for them to discuss a potential stop date with their healthcare providers when initiated on long-term PPIs. Although GERD is often a chronic condition, it may not always require ongoing acid suppression, so patients should consult their prescriber to determine if continuous PPI use is necessary or not.
What should CJ do?
Using PPIs long-term has been linked to an increased risk of various side effects. As mentioned above, studies have found mild-to-moderate association with long-term PPI use and issues like bone fractures, C. difficile infections, pneumonia, vitamin and mineral deficiencies, kidney disease, and dementia. However, since many of these side effects are uncommon, the overall risk for patients on PPIs is quite low.
CJ was prescribed Pantoprazole (a PPI) initially to help with her GERD. As time goes by, her GERD symptoms have begun to subside. She does not need to continue her PPI medication long-term. During a medication review with the pharmacist, it becomes evident that CJ should discuss with her health care provider about potentially coming off the PPI since it is no longer needed.
How to discontinue PPIs?
The American Gastroenterological Association’s Best Practice Advice Statements recommend deprescribing considerations when there is no clear indications for PPIs use. Deprescribing PPIs aims to reduce unnecessary use and long-term risks by gradually lowering the dose or frequency for patients who would benefit from it. This process should be managed by a healthcare professional to avoid rebound acid reflux. Patients should consult their physician or pharmacist before making changes to their PPI use to optimize their medication therapy management (i.e., to maximize benefits and minimize risks or side effects). Patients are also advised to regularly review their medications with their pharmacist.
Deprescribing.org has resources on deprescribing guidelines, including the Proton Pump Inhibitor evidence-based deprescribing guideline (that was published in the Canadian Family Physician, the official journal of the College of Family Physicians of Canada. It also provides a consult decision aid – “Should I Keep Taking my Acid Reflux
Medication?
Choosing Wisely Canada also has a resource titled “Bye Bye PPI: A toolkit for deprescribing proton pump inhibitors in electronic medical record (EMR)-enabled primary care settings”.
By Mona Mollaeizadeh and Certina Ho
Mona Mollaeizadeh is a PharmD student at the Leslie Dan Faculty of Pharmacy, University of Toronto; and Certina Ho is an Assistant Professor at the Department of Psychiatry and Leslie Dan Faculty of Pharmacy, University of Toronto.