By Dr. Rose Zacharias
Every day, health-care workers don masks and care for their patients. But if you could see our uncovered faces, you would see what the cumulative impact of years of unaddressed burnout looks like.
Supporting health-care workers has not been the top priority during more than two years of unprecedented strain on the health-care system. Coming out of the COVID-19 pandemic, we will call on this workforce once again to fix the gaps exposed during the pandemic while working even harder to catch up on the growing backlog of health-care services. We need to act now to ensure these workers are well enough, and provided with the supports they need, to do their jobs.
Burnout was prevalent before the pandemic. Organizations including the Ontario Medical Association have long been sounding the alarm bells on this issue. It can lead to increased depression, substance use and suicidal thoughts. It can also reduce productivity, increase turnover and possibly decrease patient access to care.
The OMA’s Physician Health Program provides confidential support to physicians struggling with substance use, mental health concerns and other behaviours. In 2021, the program saw 25 per cent higher volumes than in previous years. The complexity in cases referred for assessment in the last 18 months has also risen.
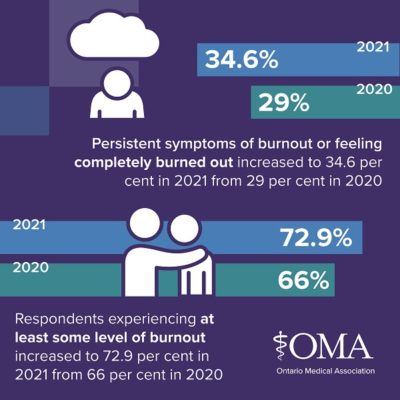 The OMA has also tracked burnout among the profession. Almost three quarters (72.9 per cent) of physicians surveyed by the OMA said they experienced some level of burnout in 2021 after one year into the pandemic, up from 66 per cent the previous year. More than one-third (34.6 per cent) reported either persistent symptoms of burnout or feeling completely burned out in 2021, up from 29 per cent in 2020.
The OMA has also tracked burnout among the profession. Almost three quarters (72.9 per cent) of physicians surveyed by the OMA said they experienced some level of burnout in 2021 after one year into the pandemic, up from 66 per cent the previous year. More than one-third (34.6 per cent) reported either persistent symptoms of burnout or feeling completely burned out in 2021, up from 29 per cent in 2020.
This is not just an Ontario phenomenon. According to the Canadian Medical Association’s 2021 National Physician Health Survey, more than half of physicians and medical learners (53 per cent) said they have experienced high levels of burnout, up from 30 per cent in 2017. As well, nearly half (46 per cent) of Canadian physicians who responded are considering reducing their clinical work in the next 24 months.
It’s important to remember that behind all these statistics are people who continue to provide excellent care for patients. It is imperative that the health system respond to this wide-reaching issue.
That’s why the OMA released a white paper identifying the top contributors to burnout and the top five solutions. Topping the list of solutions is reducing and streamlining documentation; studies have shown that physicians spend two hours on electronic documentation for every one hour of direct patient interaction.
The other top solutions are:
- More work-life balance through flexible work arrangements
- Making digital health tools a seamless part of physicians’ workflow, including by ensuring different systems can speak to each other
- Support for physician wellness at their workplaces
- Fair and equitable compensation for all work, including administrative work that cannot be reduced
Our work is not done. Finding solutions is just the beginning.
Led by the OMA’s Burnout Task Force, we are working on implementing these solutions through advocacy and collaboration with stakeholders, including the Ontario Ministry of Health. The ministry has recently joined us in making health-care worker burnout a priority by establishing a new table that is focused on solutions.
At the same time, we are exploring an interesting finding from the 2020 and 2021 member surveys on burnout. Patient interactions were the top contributors to burnout but addressing this issue did not rank as one of the top solutions in these two surveys. This is not surprising because as physicians, we take an oath to protect our patients and do no harm.
Our work to address patient interactions as a top contributor to burnout is in its early stages and includes examining issues ranging from ensuring health system capacity to meet patients’ expectations for convenient, flexible and modern options for communication and access to care, to abuse and harassment from patients and the threat of complaints and litigation. The challenge before us will be finding a solution that will positively impact the provision of care for both patients and physicians.
Nearly two and a half years into the COVID-19 pandemic, we have experienced six waves of the pandemic and have worried about caring for our patients, our loved ones and ourselves while the health-care system and the world around us were being pushed to the brink. We have had to absorb a new level of exhaustion and uncertainty, while maintaining resilience and competence at the front line.
These resources are not infinite. The challenges the health-care system is facing are piling up while the health-care workforce’s ability to fix them is dwindling.
The health-care system must heed our warnings, break down barriers and solve this crisis once and for all. Ontario’s physicians and the people they care for are depending on us.
Dr. Rose Zacharias is the president of the Ontario Medical Association. The OMA represents Ontario’s 43,000 plus physicians, medical students and retired physicians, advocating for and supporting doctors while strengthening the leadership role of doctors in caring for patients.




