By Lianne Castelino
Eyes welling with tears and voice cracking, late-night Hollywood talk show host Jimmy Kimmel recently shared a raw, intensely personal account of how the birth of his son on April 21 slipped from wonder to worry after the newborn was diagnosed with a congenital heart defect called Tetralogy of Fallot with pulmonary atresia.
The cardiac condition is the field of research of Dr. Rachel Wald, cardiologist, Peter Munk Cardiac Centre (PMCC), University Health Network (UHN). She is among several global medical experts who are part of the oldest and largest adult congenital heart disease program in the world, housed at PMCC and Toronto General Hospital, and led by Dr. Erwin Oechslin, cardiologist.
Babies born with Tetralogy of Fallot who receive care at the Hospital for Sick Children, graduate from the paediatric facility at 18 years of age. At that point, they cross the street to PMCC, where they are monitored and receive treatment as adults.
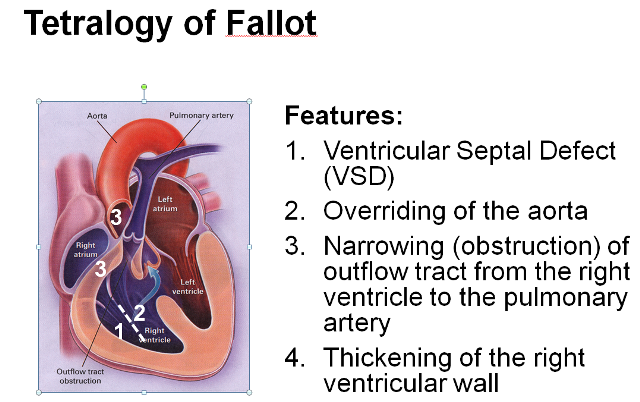
In a Q&A, Dr. Wald, describes Tetralogy of Fallot, which results from four heart defects that begin in-utero, and which require specialized life-saving surgery within the first few days of life.
Q: Describe the evolution in the diagnosis, treatment and prognosis of babies born with Tetralogy of Fallot and the timeline within which this evolution has occurred?
A: Tetralogy of Fallot (TOF) is an eponymous term describing a cluster of four congenital cardiac abnormalities which develop in fetal life. The condition occurs in 33 of 100,000 livebirths and results in decreased flow to the lungs. It is the most common explanation for a cyanotic (blue) infant.
The first breakthrough in management of this previously fatal disease occurred in 1945 when Drs. Blalock, Taussig and Thomas created a shunt to deliver augmented blood flow to the lungs. The first full surgical repair occurred in 1954. Since that time, vast improvements in pediatric cardiac surgery have translated into enhanced survival.
Today, for the first time in history, adults with repaired TOF outnumber children. At present, the diagnosis of tetralogy of Fallot is often made in fetal life, full surgical repair typically occurs at six months of age, and approximately 90 per cent of babies who are repaired can be expected to live into their fourth decade of life and beyond.
Q: What interests you most about this specific condition, your area of clinical interest and research?
A: More than any other form of congenital heart disease, TOF has seen the greatest advances in surgical management, development of percutaneous technologies and application of novel cardiac imaging applications. Despite being one of the most common forms of congenital heart disease seen by an adult congenital cardiologist and the most common condition requiring re-operation in adult life, important questions regarding the appropriate clinical management for this population remain unanswered.
One of the most critical questions to answer is when to offer pulmonary valve replacement surgery to stop complications from pulmonary valve leaking (which is a ubiquitous consequence of Tetralogy of Fallot repair in childhood). Appropriate timing of pulmonary valve replacement, as guided by cardiac magnetic resonance imaging, is the focus of my research and provides an exciting interface for various disciplines, including adult congenital and pediatric cardiology, cardiovascular surgery and cardiac imaging.
Q: Describe the expertise that PMCC has in this area?
A: At the Peter Munk Cardiac Centre, unparalleled clinical strengths have allowed us to create global research programs. Given our adult congenital cardiology program, which is among the largest in the world, and our congenital cardiology cardiac magnetic resonance imaging volumes, which are the largest in Canada, we have successfully created the world’s largest prospective registry of children and adults with Tetralogy of Fallot with contemporary cardiovascular magnetic resonance imaging which is entitled CORRELATE (Canadian Outcomes Registry Late After Tetralogy of Fallot Repair). A Canadian Institutes of Health Research-funded study, it currently has close to 650 participants in Canada, Europe and Asia.
Lianne Castelino is a Senior Public Affairs Advisor at Peter Munk Cardiac Centre, University Health Network.