By Dale Mayerson and Karen Thompson
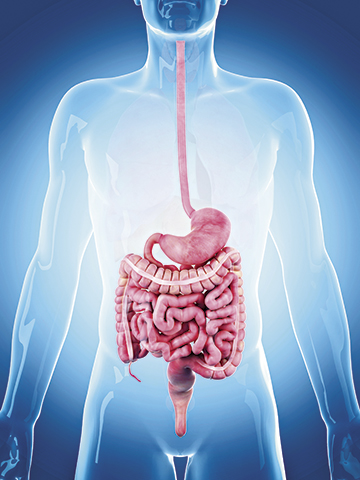
The digestive system is a complex series of structures that use food to fuel and strengthen the body. It is one continuous tube from the Assessing residents for chewing, swallowing, digestive problems, and any other reason for poor intake at meals and snacks, is the first step in setting up individualized interventions.
mouth to the anus, and reaches approximately nine metres (30 feet) in length. The goal of the digestive tract is to thoroughly break down the food we eat in order to extract the nutrients that keep us healthy.
The digestive system starts with the mouth, where food is chewed. The four different shapes of teeth help to grind, shred and tear food into small pieces in preparation for swallowing. Saliva mixes with food to moisten it and an enzyme in the saliva starts to break down starches. The tongue creates small masses of chewed food and moves them to the back of the throat in preparation for swallowing.
The esophagus moves food from the throat to the stomach. There are small seals at each end of the esophagus called sphincters, that open and close in response to movement of food through the system.
In the stomach, food particles break down due to the hydrochloric acid and enzymes produced in the stomach lining. The stomach also mechanically churns to help this process along. The acid is especially effective on proteins that need to be completely dismantled into amino acids before they can be absorbed into the blood stream. It takes about six hours for food to move through the stomach, although the timing can be affected by the amount of fat as well as the amount of fibre in the food. The resulting mixture moving out of the stomach is a wet, partially dissolved mass, ready for the next step in the small intestine.
Although this is a marvellous process, there are many possible “glitches” in the system, and problems develop more frequently with aging. The following is a list of just some of the disorders and conditions of the upper digestive tract:
Periodontal disease – Poor oral health, lack of brushing, flossing and regular dental check ups can cause gum disease, leaving teeth loose and damaged. Gingivitis is inflammation of the gums, caused by bacteria building up in plaque, and the more serious periodontal disease causes the inner layer of the gum and bone to be slowly destroyed. This can lead to extreme pain and poor food intake, ultimately requiring tooth removal and the need for dentures. Teeth in poor condition may be sensitivie to very hot or very cold foods. There is evidence that bacteria in the mouth, resulting from poor oral health, has been associated with heart disease and dementia, and can make diabetes worse.
Saliva flow – We produce up to a litre of saliva per day, but saliva may be reduced with aging, making it more difficult to moisten food while chewing and swallowing. Less saliva also makes it more difficult to taste food, possibly affecting the person’s overall food and nutrient intake. Medications can cause side effects such as dry mouth, leading to tooth damage. Dry mouth is medically termed xerostomia.
Denture use – Dentures must fit correctly over the gums, to avoid rubbing and irritation that can lead to open sores. Dentures must also be cleaned regularly and frequently, to avoid food particles being trapped in the dentures or between the dentures and the gums. Food particles that are swallowed hours after eating can lead to symptoms of food poisoning.
Dysphagia – Swallowing disorders can cause food to land in the trachea – the tube leading to the lungs, instead of going into the esophagus. Even though swallowing can take just a second or two, more than 50 muscles are involved. Dysphagia is often a result of dementia, stroke, Parkinson’s disease and other medical conditions, such as cancer of the throat. Food may need to be pureed to a smooth homogeneous texture, to make it as safe as possible to swallow.
Reflux – Also known as heartburn, this is a problem with the lower sphincter of the esophagus. The highly acidic environment of the stomach can splash up into the esophagus if the sphincter is not tightly closed, causing pain or a burning sensation. This can be an occasional occurrence, but if it is an ongoing problem, it is better known as GERD – gastroesophageal reflux disease. Advice for reflux includes: eating smaller meals, avoiding caffeine and spicy foods, and sitting up for 30 to 60 minutes after eating. There are many antacids and other medications that help to relieve this problem.
Like all systems in the body, the digestive system gradually ages in its functioning, causing changes that can affect eating and nutrient intake. Due to dental problems, many residents in long-term care can no longer chew hard foods or thick, solid pieces of meat. For some frail seniors, even the act of chewing and swallowing can be tiring, so a softer texture increases the opportunity for intake of more nutrients in a meal. Foods that are easier to digest still need to have substantial protein and other nutrients.
Some seniors feel a loss of appetite, possibly due to reduction in the taste or smell of foods. This can be made worse with some medications. It is important to assess residents to ensure that they are able to get everything they need nutritionally from their meals before turning to liquid oral nutritional supplements. In long-term care, this is becoming known as the “food first” philosophy. Poor food and fluid intake can lead to a whole host of problems such as: frailty, unwanted weight loss, skin breakdown, greater risk of falls, and more. Assessing residents for chewing, swallowing, digestive problems, and any other reason for poor intake at meals and snacks, is the first step in setting up individualized interventions.
Seniors in long-term care greatly benefit from consistent daily oral care and visits with a dentist and denturist as required. Residents also need a quick resolution to gastrointestinal problems and complaints, with interdisciplinary team involvement – doctor, nurse, dietitian and front line staff all doing their parts to ensure that residents are eating and drinking, and for best quality of life.
Dale Mayerson, B Sc, RD, CDE, and Karen Thompson, B A Sc, RD are Registered Dietitians with extensive experience in Long-term care. They are co-authors of “Menu Planning in Long Term Care and Retirement Homes: A Comprehensive Guide” and have participated for many years on the Ontario Long Term Care Action Group, an advocacy group of Dietitians in Canada.