By Dr. Janice Mann
Chronic pain. It’s one of the most common reasons we visit a doctor or other health care professional. And, until recently, it wasn’t uncommon to leave their office with a prescription for an opioid painkiller in hand. Opioids are a class of drugs that are prescribed to treat pain, and include codeine, fentanyl, oxycodone, and morphine. However, the drawbacks and risks of these commonly prescribed medications are becoming increasingly recognized.
Opioids, in addition to treating pain, can also result in a feeling of euphoria or a “high.” And stopping the medication can cause unpleasant withdrawal symptoms. As a result, some people who have been prescribed opioids for pain can become addicted to the medication. Prescription opioids can also be misused in a variety of ways; they may be taken by someone else, taken at a higher dose than intended, taken in a different way than prescribed (i.e., injected rather than taken by mouth), or combined with other drugs or alcohol.
The potential for addiction or misuse combined with a long list of possible side effects — including coma and death in the case of overdose — have led the health care community and patients in Canada to seek alternatives to opioids for safely and effectively treating chronic pain. In fact, the 2017 Draft Recommendations for Use of Opioids in Chronic Non-Cancer Pain from the National Pain Centre at McMaster University recommend optimization of non-opioid pharmacotherapy (medications other than opioids) and non-pharmacological therapy (treatments that aren’t medications), rather than opioids for patients with chronic pain.
But what treatments — other than opioids — are available for chronic pain? And more importantly, how do we know if they work?
That’s where CADTH — an independent agency that finds, assesses, and summarizes the research on drugs, medical devices, tests, and procedures — can help. Recently CADTH was asked to look at the evidence on a treatment for chronic pain that doesn’t involve any medication and that patients can use in their own home, called transcutaneous electrical nerve stimulation or TENS.
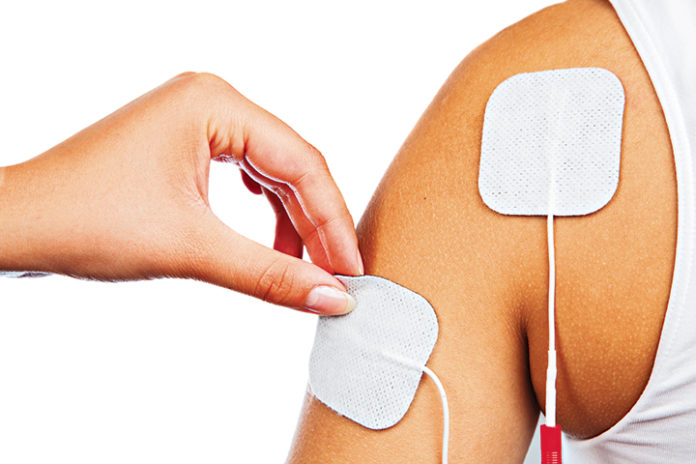
With TENS, electrodes are placed on the skin around the area of pain. The area is then stimulated with low-voltage electricity usually for 30 minutes up to an hour, twice each day. Traditionally TENS has been provided by a health care provider in a clinic setting. However, TENS is now commonly available for home use. While using TENS at home can be more convenient for patients, whether it is effective in this setting hasn’t been clear and purchasing the devices can be expensive for patients and their families. That’s why CADTH was asked to assess the evidence and shed some light on the usefulness of home-based TENS for chronic pain.
After a careful search for evidence, CADTH found four clinical studies and five evidence-based guidelines that were best suited to help answer questions about how well TENS in the home may work to treat chronic pain. Unfortunately, it wasn’t a lot of evidence to go on, and questions about TENS in the home still remain. For example, the studies showed mixed results about whether home-based TENS improved chronic pain. And no studies compared home-based TENS with drug treatment options such as opioids. Guidelines did not recommend TENS for osteoarthritis of the knee, chronic neck pain, or chronic low back pain (although these weren’t specific to home-based TENS). Two guidelines did recommend that home-based TENS be purchased to treat chronic pain only if TENS in a clinic setting had already been tried and proved to be effective for that patient.
So what does this tell us? It means that we aren’t really sure how effective TENS in the home may be for chronic pain. The available evidence doesn’t prove that it works, but it also doesn’t prove that TENS in the home does not work. And that means we need more evidence.
TENS in the home is just one example of a health technology that may be considered for the treatment of chronic pain. And it’s a good example to remind us that we need to look at the evidence before jumping to alternatives to opioids to treat pain. As the push to find effective and safe alternatives to opioids to treat chronic pain continues to grow, the need for high-quality evidence on these alternatives will also increase. With the evidence in hand, health care decision-makers — including health care providers and their patients — can make informed decisions about the safe and effective treatment of chronic pain.
CADTH is committed to ensuring that all decision-makers have the evidence they need on alternatives to opioids for the treatment of chronic pain. To learn more, visit www.cadth.ca/opioids or speak to a CADTH liaison officer in your region.
Dr. Janice Mann, Bsc, MD is a Knowledge Mobilization Officer at CADTH.