By Nicole Forget and Stacey Palangio
Fall marks the time of year when Canada’s most entrepreneurial physicians are recognized and celebrated, all in the name of health care innovation. For the third year, Joule’s Innovation grant program shines a light on some of Canada’s most impressive innovations and those who dared to imagine them.
The grants, which total $200,000 in flexible funding, are open to all the Canadian Medical Association’s 87,000 plus members. Along with early and later stage innovations, Joule’s grants support social innovations―initiatives that address a societal problem in a manner that improves the status quo, and for which the primary value created is to health care as a whole. This year, Joule widened the playing field by adding four new grants specifically aimed at medical students and residents.
Of 183 exceptional submissions, nine were chosen based on four weighted criteria: health care benefits, degree of disruption, relevance and scalability. The range of technology-driven solutions address a wide scope of issues ranging from gaps in quality of care and accuracy of diagnostics to clinician experience and training the next generation of physicians.
Each of Joule’s nine 2018 grant recipients will use the grant funding to take their ventures to a new level and drive change in Canada and beyond.

Conavi Medical―Improving tools, improving outcomes
Open surgical procedures are becoming increasingly less common and are being replaced by minimally invasive techniques―however existing imaging modalities are often limited―in terms of visualization capabilities such as field of view, contrast and resolution, as well as cost and deliverability to anatomic targets.
To address these limitations, Dr. Brian Courtney and his team founded Conavi Medical, a medical device company that develops image guidance technologies for use in minimally invasive procedures. The company’s primary product offering is an intravascular imaging system, which combines catheter-based intravascular ultrasound (IVUS) and optical coherence tomography (OCT) onto a single catheter for use in coronary arteries. This system is the first technology to combine co-linear and co-registered IVUS and OCT, and the cost, image quality and catheter-size are comparable to standalone systems.
Ultimately, Conavi’s goal is to be the world-leading provider of image guidance technologies for use in minimally invasive procedures so that they may be simpler, faster, safer and more cost-effective.

Careteam Technologies ―A holistic approach to patient care
Care fragmentation is a challenge in our current health care system. It is a headache for patients, families, providers and the whole care team, often resulting in poor outcomes.
Dr. Alexandra T. Greenhill, physician turned tech entrepreneur, sought to address this gap by developing Careteam Technologies, a flexible communication tool focused on the patient and their support circle. An AI-enhanced digital health platform, Careteam enables patient-centered care collaboration and system navigation for patients, especially those with complex, chronic diseases. Working across different health conditions and contexts including hospital, clinic, community and home, the platform works to make sure everyone involved is on the same page―patients, families and health professionals.
As a whole, this collaborative platform reduces system costs and improves outcomes while increasing both patient and provider satisfaction―benefitting the quadruple aim.

Critical Outreach & Diagnostic Intervention (CODI)―Better care in rural and remote areas
Rural physicians are often faced with critical situations where they need additional support they simply can’t access. As a result, patients may get suboptimal care, rural physicians will get discouraged and exit the community, leaving many patients without a physician.
To support rural physicians, Dr. Donald Burke and his team developed a service app called Critical Outreach & Diagnostic Intervention (CODI). CODI provides an on-demand, virtual 24/7, immediate point of care service that connects rural physicians and intensivists in British Columbia. They can communicate via audio and video, even in areas of poor connectivity or reception.
The CODI app aims to improve the confidence and skills of rural physicians to increase both their recruitment and retention―leading to better patient outcomes, fewer unnecessary hospital transfers and reduced health care costs.

Aifred Health―Harnessing AI for better mental health treatment
Depression is common, affecting over 300 million people worldwide. Despite the treatments available, clinicians often require multiple attempts before identifying an effective treatment for their individual patients.
Aifred Health, a company led by Dr. David Benrimoh, has developed a clinical decision aid as a response―harnessing the power of artificial intelligence (AI) to more accurately recommend optimal treatment for patients with depression. By training computer algorithms with evidence-based medical data to produce treatment decision aids, Aifred Health is supporting physicians to prescribe treatments more effectively.
By way of precision medicine, Aifred Health aims to enhance the quality of mental health care services by improving patient flow and reducing patient recovery time, health care costs and clinician burnout.

My On Call (MOC) Pager App―A learning tool to support clinical excellence
It’s estimated that 138,000 Canadians suffer adverse events due to medical errors each year, of which approximately half involve errors in clinical decision-making.
To address this challenge, resident physician Dr. Nada Gawad led the development of the My On Call (MOC) Pager App. As a real-time simulated pager program, it is designed to practice safe clinical decision-making. The MOC Pager App serves as a unique adjunct to clinical training and addresses the currently unmet need to practice and assess clinical decision-making across any discipline or stage of training.
As the first and only simulated pager app, the MOC Pager App pushes the boundaries of technology in health care to support clinical excellence. Their ultimate goal is to improve patient safety.

16 Bit―Using data-driven intel for system efficiency
Approximately one in eight women will be diagnosed with breast cancer in their lifetime. Mammograms are the current gold-standard for screening and are recommended on a biennial basis for women aged 50-74 in Canada. However, the majority of screening mammograms are normal or benign.
Resident physician Dr. Alex Bilbily and his company, 16 Bit, undertook this challenge by developing the Intelligent Mammogram Triage System, capable of triaging screening mammograms with high negative predictive value. Through this initiative, should a mammogram be deemed normal or benign by the artificially intelligent system, a radiologist interpretation may no longer be required.
Such a system will decrease the cost associated with screening programs and the burden on radiologists, providing a means of creating widespread screening programs that are economically feasible.

Stand Up for Health (SU4H) ― A learning simulation for the social determinants of health
The common didactic approach to teaching can often leave learners with a superficial understanding of concepts such as the social determinants of health.
Stand Up for Health (SU4H) is a not-for-profit organization―led by resident physician Dr. Latif Murji―that aims to use experiential learning to generate meaningful discussion and action surrounding the social determinants of health. Its cornerstone is an immersive simulation that places participants in the role of Canadians living in poverty. Participants interact, make choices, and solve challenges within their given set of circumstances. The workshop concludes with a facilitated discussion on public policy and the challenges marginalized Canadians face.
SU4H will redefine the field of medical education by shifting didactic teachings to an interactive, technology-based simulation for physicians and trainees, leading to a healthier and more equitable society.
Lumina―Reducing risk through efficiency
Lumina, created by fourth year medical student Eric J. Zhao and his team, is an improved Toolkit for Central Line Access. The Lumina team―which consists of engineers, students, and physicians including Dr. David Agulnik―is driven by a shared belief in improving health outcomes for Canadians through evolutionary design. Its creation was catalyzed by the support of the medtech community in Vancouver and the University of British Columbia.
The device combines the tools for needle insertion, flashback verification, and guidewire insertion into one compact, ergonomic tool. With Lumina, the user can advance the guidewire immediately after flashback. The team has also designed a simple modification to existing dilators―a slit running down the entire length of the dilator―that allows the dilator to be snapped onto the guidewire anywhere along its length. This decreases the travel distance and risk for compromise of sterility when working with long guidewires.
Lumina is committed to finding simple solutions to tough problems. This tool will enable physicians to have more control in ER scenarios, helping them perform at their peak performance and provide excellence in health and patient care.

VitalEyes―Extending care to the waiting room
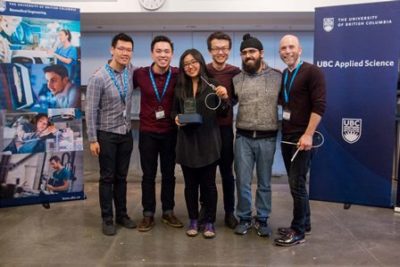
VitalEyes was created by medical student Charles Choi and his team at Hatching Health, a weekend hackathon with students and professionals in technology and health care. Inspired by Dr. David Agulnik’s experiences in the Emergency Department at St. Paul’s Hospital, the team worked to develop a prototype.
VitalEyes simultaneously measures heart rate, respiratory rate, and temperature of a single patient. The potential of their work has been recognized by the Faculty of Applied Sciences Award at Hatching Health. They also received the finalist award at RBC Get Seeded and were semi-finalists for Medical Device Development Centre’s Award for Excellence in Biomedical Engineering.
Recently, their team has expanded, and they are exploring the use of video cameras, 24GHz frequency modulated continuous wave radars, and thermographic cameras to determine heart rate, respiratory rate, and temperature. Their system is designed to then alert healthcare professionals to attend to deteriorating patients whose vital signs have become abnormal.
These are nine of the hundreds of physicians who are leading by example, forging the pathway to better health. Joule is proud to boost their efforts as they improve the health care landscape in Canada and internationally. At the same time, we’d like to thank them for reminding all of us that when it comes to physician-led innovation, the possibilities are truly endless. We can’t wait to see what the future holds for each of them.
To learn more about the Joule Innovation grant program, each recipient and to prepare for 2019, visit joulecma.ca/grants.
Have an innovation you think Joule should support? Consider applying to the program next year.
Nicole Forget is Content Manager and Stacey Palangio is the Contract Writer at Joule Inc.


