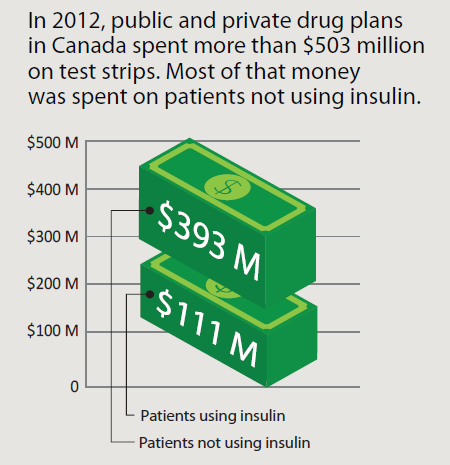
Type 2 diabetes is a growing epidemic with significant implications for Canadians and the Canadian health care system. One aspect of diabetes management that has recently come under scrutiny is the practice of self-monitoring of blood glucose (SMBG). The test strips used for SMBG represent one of the largest expenses in diabetes management, with some estimates showing that more money is spent on test strips than on all oral antidiabetes medication combined. Recently, several public drug plans in Canada have made changes to their reimbursement policies surrounding test strip coverage. What do these changes mean for patients, and what does the evidence show?
Assessing the evidence
In 2009, The Canadian Agency for Drugs and Technologies in Health (CADTH) performed a systematic review of randomized controlled trials (RCTs) and observational studies comparing SMBG with no SMBG, or comparing SMBG frequencies. Meta-analyses were conducted to pool trial results, when appropriate. The results are summarized as follows:
Patients with type 2 diabetes using insulin—studies were few and of low quality, but evidence suggests that SMBG is associated with improvements in glycemic control, as measured by a change of approximately -1% in haemoglobin A1C from baseline.
Patients with type 2 diabetes not using insulin but using oral antidiabetes drugs (e.g., metformin)—SMBG resulted in a pooled A1C difference of -0.25%, which is statistically significant but not considered clinically significant.
Patients with type 2 diabetes who do not take any antidiabetes drugs—SMBG resulted in a pooled A1C difference of -0.05%, which is not statistically or clinically significant.
ANTI-INFLAMMATORY DRUGS: WHAT’S THE EVIDENCE?
For all patient groups, there was little or no evidence to suggest that SMBG improves patients’ quality of life, satisfaction, and body weight. Longer term studies are needed to determine whether SMBG reduces long-term complications of diabetes or mortality, and more research is also needed on the effect of SMBG in gestational diabetes.
The cost-effectiveness analysis found that SMBG performed nine times a week in patients not using insulin was associated with an incremental cost of $113,643 per quality-adjusted life-year (QALY) gained, relative to no SMBG. This cost exceeds commonly accepted thresholds, which means that SMBG for this group is not cost-effective.
Recommendations
A panel of experts developed recommendations based on the CADTH findings.
For patients using insulin, the panel recommends that SMBG should be individualized to guide adjustments to insulin therapy. In adults with type 2 diabetes using basal insulin, SMBG up to 14 times a week should suffice in most cases.
For most adults with type 2 diabetes not using insulin, the panel recommends that routine SMBG is not required. Therefore, patients managing their type 2 diabetes using oral antidiabetes medication, diet, or exercise do not need to self-monitor their blood glucose as frequently, and this will not negatively affect their health.
MORE: NEW TREATMENT OPTIONS FOR MUTLIPLE SCLEROSIS
The panel notes that every once in a while, short-term testing may be helpful for patients if they are experiencing unstable glucose levels, acute illness (e.g., flu), if they are pregnant or trying to become pregnant, or if they are changing their medication or routine (e.g., travelling). More frequent testing can also benefit patients who are at higher risk of hypoglycemia because of inadequate diet, unforeseen exercise, history of severe hypoglycemia or hypoglycemic unawareness, or if they are taking medications that carry a higher risk of hypoglycemia, such as drugs in the sulfonylurea class (e.g., glyburide, gliclazide, glimerpiride).
Testing for a reason
It is important to keep in mind that SMBG is only as useful as the action it triggers, whether that means adjusting insulin dose, taking glucose, changing diet, or finding motivation to exercise more. It’s these changes that lead to better glycemic control—not the act of SMBG itself. In other words, most patients with type 2 diabetes will benefit more from focusing on other aspects of diabetes self-management. Testing their blood glucose less often will not negatively affect their health, and it will free up time and resources.
CADTH calculated that if these recommendations are put into practice and patients who don’t use insulin tested less often, more than $260 million could be freed up each year for spending on other health technologies. This is an important consideration when operating within a health care system that has finite resources.
To read more about SMBG, visit www.cadth.ca/smbg