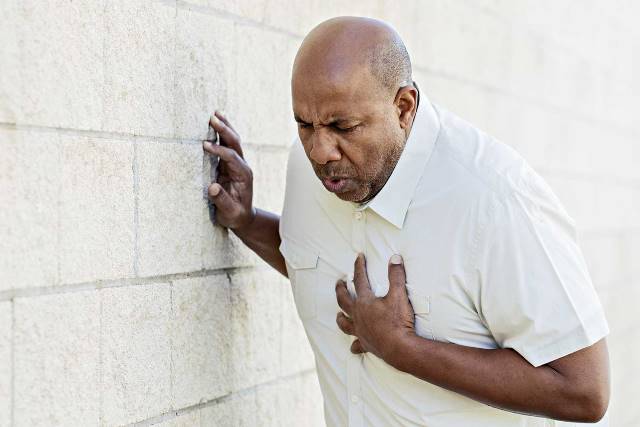
If the person sitting beside you suddenly developed #chest pain, how would you know if they were having a #heart attack? What if it was indigestion? Or muscle pain? Or even pneumonia? Health care professionals face this same dilemma every day in health care settings across the country. And when it comes to saving heart muscle, heart function, and patient lives, figuring out whether or not chest pain is caused by a heart attack – a sudden lack of oxygen to the heart – is crucial.
Fortunately, in addition to the clinical exam, health care professionals have some tools of the trade that can help them determine the cause of a patient’s chest pain. An electrocardiogram or ECG can help, but while some heart attacks lead to typical changes on the ECG, others do not. That’s why clinicians also rely on blood tests. One of these tests measures the amount of a biomarker in the blood called #troponin. If the heart isn’t getting enough oxygen – which is the case during a heart attack – heart cells die. These damaged cells release troponin into the blood stream. Higher-than-normal levels of troponin indicate that it’s likely that the patient is having a heart attack; lower or normal levels of troponin suggest that the chest pain may be due to something else. And although troponin testing can be very helpful in determining the cause of chest pain, it isn’t perfect. Some other medical conditions – like kidney failure or neuromuscular diseases – can also lead to higher than normal troponin levels.
One of the biggest challenges of troponin testing, however, is its availability. In the past, testing such as this could only be performed in a central laboratory. While this isn’t an issue for larger hospitals with 24-hour lab service, rural hospitals or remote locations do not always have ready access to lab services. In these settings, labs may not be located on site or, if they are, might not be open 24 hours a day. Lack of availability of troponin testing in rural hospitals and remote settings leaves clinicians without one important source of information when determining the cause of their patients’ chest pain.
MORE:Personalized medicine: Is Timothy Caulfield right about everything?
But there is a way that troponin levels in the blood can be measured without the need of a central lab. Point-of-care troponin testing is a care model that moves the test to the patient rather than sending the patient’s blood sample to the lab. There are several point-of-care troponin devices – either handheld or desktop models – available in Canada. And these tests can give troponin results in 10 to 20 minutes (the recommended time for labs to give troponin testing results is an hour or less). Having access to troponin results could help health care providers in rural hospitals and remote locations better determine who really does require a transfer to a larger health centre for more testing and advanced care and who can safely remain in their community for local care.
As the devices are starting to be used across Canada, a number of questions about how well they work and in which health care settings they should be used have come up. To answer these questions, the health care community turned to CADTH — an independent agency that finds, assesses, and summarizes the research on drugs, medical devices, tests, and procedures — to find out what the evidence says. CADTH gathered the evidence from medical research on point-of-care troponin testing for patients with chest pain, which was then used by an expert committee to make recommendations for its use in the Canadian health care system.
The evidence on point-of-care troponin testing shows that how well the test works can vary quite a lot. And whether it offers good value for money can really depend on many different factors, including the setting in which it’s used. The evidence does suggest that point-of-care troponin testing can reduce the turnaround time from taking the test to having the results, may shorten the time a patient spends in the emergency room, and may lead to a quicker diagnosis and treatment decision. However, whether this results in meaningful differences to patients or their health isn’t clear. Although the evidence about using point-of-care troponin testing in health care settings without access to a central lab is limited, it suggests that referrals and transfers from a rural hospital or remote setting to larger health care centres can be reduced by this type of testing, and that use in ambulance settings may be beneficial.
MORE: DEPRESSION IN THE ELDERLY: WHERE’S THE EVIDENCE?
The recommendation of the expert committee, based on all these findings, is to use point-of-care troponin testing in health care settings where immediate access to a central lab is not possible. On the flip side, if lab troponin testing can be readily accessed, point-of-care troponin testing is not recommended.
Used in this way, point-of-care troponin testing can help to ensure that all patients (and their health care providers) can benefit from troponin results when determining the cause of chest pain. Those patients likely to be experiencing a heart attack can be transferred to a larger centre for more testing and advanced cardiac care. Those patients who are likely not experiencing a heart attack can remain in their community and be cared for locally – minimizing unnecessary transfers and disruption to patients and their families.
If you’d like to learn more about CADTH’s project on the point of care troponin testing for patients with chest pain, visit www.cadth.ca/POCtroponin. And if you would like to learn more about CADTH and the evidence it has to offer to help guide health care decisions in Canada, please visit www.cadth.ca, follow us on Twitter @CADTH_ACMTS, or talk to our Liaison Officer in your region: www.cadth.ca/contact-us/liaison-officers.