
Shaf Keshavjee and Marcelo Cypel continue to see the future for the Ex-Vivo Lung Perfusion (EVLP) System they invented.
Having reached the 1,000th procedure of the EVLP – a milestone occurring more than a decade after its inception – they see nothing but monumental outcomes for lung transplantations at UHN and around the world.
“I saw the 1,000th coming, and I see the 10,000th coming,” Dr. Keshavjee, Chief of Innovation at UHN and co-creator of the homegrown EVLP, says of the system, which was invented in 2008, became a fully approved and funded clinical therapy in 2011, and marked its 1,000th procedure just last month.
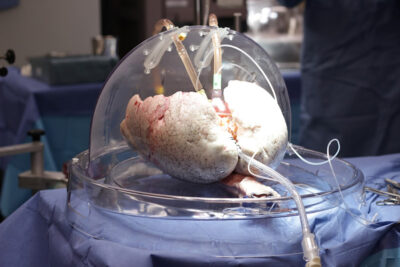
The EVLP maintains donor lungs outside the body by mimicking body temperature and providing nutrients prior to transplantation, resulting in increased lung health and lower rates of rejection following the surgery.
The milestone transplantation surgery for the EVLP was performed in March on one of about 1,400 patients in Ontario currently awaiting an organ transplant. The patient’s information cannot be disclosed to protect privacy, but the number itself speaks volumes to the utility of the procedure.
“This is significant because it really shows how much this technique has matured, and that it has a strong track record of benefiting those needing a lung transplant,” says Dr. Cypel, Surgical Director of UHN’s Ajmera Transplant Centre and staff thoracic surgeon at UHN, and a professor in the Department of Surgery at the University of Toronto.
“I don’t think we’d get to 1,000 procedures in any surgical procedure without seeing the striking benefits it’s bringing to patients,” he says.
The EVLP System was developed at UHN but has since been recognized and implemented internationally.
It’s now used across five continents, including leading transplant centres in the United States such as Duke University Hospital, Cleveland Clinic, Mayo Clinic, as well as Europe, South America, Asia, Israel and Australia, with the highest volume of transplants occurring in the U.S.
“UHN has invented a new solution, and just as important has assisted in its development into a commercial product that can now be applied and implemented at transplantation sites around the world,” says Dr. Brad Wouters, Executive Vice President of Science and Research at UHN.
“It’s a good example of translation of research to benefit patients here at UHN and around the world, identifying unmet patient needs, which is what our physicians here are experts at doing,” he says.
The Toronto General Hospital Research Institute (TGHRI) – the research arm of Toronto General Hospital – is one of top medical research programs worldwide, supporting the medical programs of the hospital with multidisciplinary experts in the fields of organ transplantation, regenerative medicine, cardiology, diabetes and infectious diseases, among others.
TGHRI is home to more than 150 scientists and clinicians who work together to bring innovative research findings from the lab directly to patients, with notable findings including the first clinical use of insulin and the first cardiac pacemaker, among many other novel approaches, including EVLP.
The EVLP System can be used to make the donor lungs look more like the recipient’s, resulting in increased lung health prior to transplantation, higher chances of donor matches and lower rates of rejection following the surgery.
Prior to this system, 80 per cent of donated organs went unused because the lungs did not meet standard acceptance criteria.
“People sign up to become organ donors assuming they’re going to donate their organs, when in reality, the majority of lungs around the world are not used because [medical professionals] can’t be sure that they’re safe for transplantation,” says
Dr. Keshavjee.
Dr. Keshavjee and Dr. Cypel’s development poses a monumental change for patients waiting for an organ transplant and has more than doubled the number of clinically acceptable lung donations at UHN.
“[EVLP] allows people who choose to be organ donors to be sure that their lungs are going to be successfully donated,” says Dr. Keshavjee.
“Over 40 per cent of donated lungs in Toronto are now able to be used for transplantation, whereas before only 20 per cent were utilized,” he says.
The Toronto Lung Transplant Program in UHN’s Ajmera Transplant Centre at Toronto General Hospital is the largest and most successful lung transplant program worldwide. It was the first centre in the world to perform both a single (1983) and double lung (1986) transplant and in 2008, conducted the first human EVLP surgery to repair and recondition donor lungs prior to transplantation.
UHN’s Sprott Department of Surgery is the largest surgical program in Canada, spanning 13 surgical divisions – from cardiovascular to neurosurgery to thoracic – across three UHN hospitals: Toronto General Hospital, Toronto Western Hospital and Princess Margaret Cancer Centre.
In 2020, a UHN team of transplant surgeons, led by Dr. Keshavjee, were awarded a $24-million New Frontiers in Research Fund (NFRF) grant from the CIHR and the federal government to further advance ex-vivo transplant technology, including repairing and rebuilding other organs outside the body. This team also received support from UHN Foundation, whose donors have been supporting the development and evolution of EVLP since its very early days.
Both Drs. Keshavjee and Cypel continue to work towards advancing the future and clinical potential of ex-vivo perfusion. Recently, Dr. Cypel and his team used EVLP to modify organ blood type to universal type O blood organs (universal blood type) for transplantation.
“This could have a dramatic change in how we currently allocate organs for transplant,” says Dr. Cypel.
“EVLP is ultimately a platform that allows us to do more sophisticated things,” says Dr. Keshavjee, who believes it’s just the beginning for ex-vivo perfusion – and will be the future of all organ transplantation, whether it’s the kidney, pancreas, lungs or the heart.
By Catherine Danko
Catherine Danko works in communications at UHN.

