By An Tang
The disruption created by COVID-19 has created an opportunity to consider modernization of the patient journey through the healthcare system. Technology “appification” and the improvement of the patient experience through the integration of technology could turn our current structure into a streamlined, paperless, patient-oriented system designed for the 21st century.
Appification refers to the use of programs running on mobile devices to provide a user-friendly interface to enter and consult data available on the web or from medical databases. Apps can facilitate patient access and integration with radiology departments but will require overcoming communication, technical, and security barriers encountered in medical imaging. Achieving seamless integration of databases within and between radiology departments will require adoption of open architectures and communication standards by providers of medical databases.
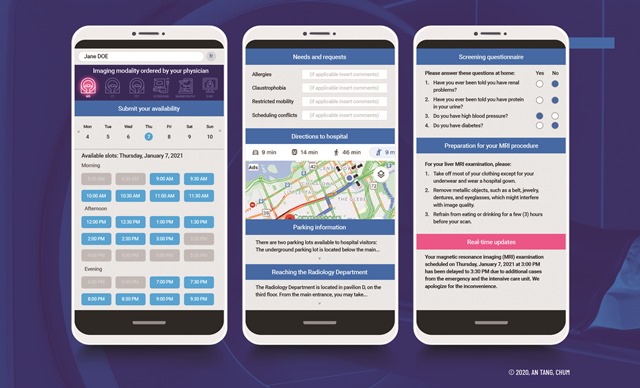
Dynamic scheduling apps with real-time notifications can reduce idle time in radiology departments and eliminate the need for crowded waiting rooms. Patients, in consultation with referring physicians, may be able to:
- Access necessary imaging services through the web or an app
- Note special needs (e.g. allergies, claustrophobia, restricted mobility, scheduling conflicts)
- Allow referring to match level of examination priority with the scheduling availability of the department based on wait times
- View the impact of special requests on availability
- Inform radiology departments of arrival delays
- Receive notifications and status updates by phone, in the event of a schedule change
- Access information on parking or how to reach the radiology department
- Receive real-time updates on the progress and reporting status of their imaging study
Ultimately, appification will allow patients to remain informed and empowered. The implementation of tools that provide more updated information and demystify a needlessly complex patchwork of services, providers, and protocols will greatly improve the patient experience. In the future, patients need not be subject to overbooking, lack of granularity in scheduling, or the disempowerment and anxiety that may result from a lack of information regarding their tests and appointments.
The patient journey through a radiology department is a process that can be greatly improved with enhanced use of technology and apps. For historical reasons, some of the steps – such as requisitions for outpatients and printed preparation instructions – are still paper-based or reliant on faxed copies even when the information is available in digital formats. The Simplified Patient Journey figure illustrates existing processes (in gray) and areas for targeted improvement (in blue) from scheduling and image acquisition through to reporting and subsequent integration with multi-disciplinary care. While all documents are already available in digital format, there is still a propensity to print and mail screening questionnaires and preparation forms. Even for steps that are entirely digital, there is room for improvement with respect to how we link existing systems and information.
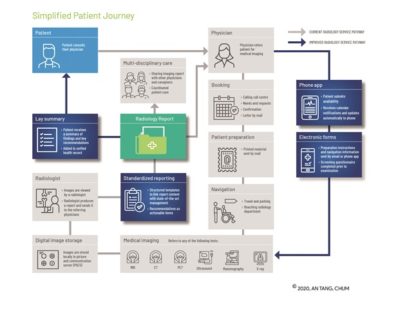 Complete digitization of the patient workflow has the potential to shorten delays between each step, facilitate automation of repetitive tasks, reduce clerical errors, and enable the use of optimization algorithms and artificial intelligence for image analysis. From the patient’s perspective, thoughtful integration of technology into the process can improve the overall experience. For example, patients will be able to share their needs and requests, complete screening questionnaires, and read preparation instructions remotely and ahead of their examinations. These steps are important to prevent the late discovery of a contraindication to an imaging examination that may further delay appropriate imaging. With cell phone applications, patients may receive geolocated information (such as guidance on waiting location to reduce patient density according to social distancing requirements) and real-time updates (such as potential delays due to medical emergencies).
Complete digitization of the patient workflow has the potential to shorten delays between each step, facilitate automation of repetitive tasks, reduce clerical errors, and enable the use of optimization algorithms and artificial intelligence for image analysis. From the patient’s perspective, thoughtful integration of technology into the process can improve the overall experience. For example, patients will be able to share their needs and requests, complete screening questionnaires, and read preparation instructions remotely and ahead of their examinations. These steps are important to prevent the late discovery of a contraindication to an imaging examination that may further delay appropriate imaging. With cell phone applications, patients may receive geolocated information (such as guidance on waiting location to reduce patient density according to social distancing requirements) and real-time updates (such as potential delays due to medical emergencies).
Imaging will be combined with other specialist appointments and next-step referrals to streamline the patient experience. Doing so will also expedite imaging for screening and follow-up. This would lead to seamless sharing of reports and actionable items by radiologists to referring physicians and other professionals involved in multi-disciplinary patient care. For patients who are eligible for screening according to practice guidelines, reminders to book imaging appointments can be made. These reminders may be sent by email, text messaging, notifications via the phone application, or by access through a patient results portal.
In the future, we envision patients at the center of the feedback loop. Patients should be able to access all results, including their medical images and reports, from a unified portal that can be accessed from any clinic or hospital, and across provincial jurisdictions. Communication will be two-way, so that patients can upload their own data such as photographs of how a scar is healing. Establishing appropriate data protection and safety nets will be essential to this evolution, so that parents/guardians can access results on behalf of their dependents where necessary, and to ensure patients receive their results in an environment where they have the opportunity to ask follow-up questions and receive guidance from their physician.
It is our vision that artificial intelligence and digital applications will be harnessed to improve the patient experience and prepare for a better future.
An Tang, MD, MSc, FRCPC is a Full Clinical Professor, Radiology Department, Université de Montréal.