Imagine waking up one morning with symptoms often associated with heart attacks: shortness of breath, pain in the chest or back radiating down the arm. These are alarming symptoms that without question would send someone to the emergency room immediately. But for the majority of people, getting winded at the top of a flight of stairs or aches and pains in the lower legs are the symptoms that people tend to endure or ignore – symptoms of coronary artery disease (CAD) or peripheral artery disease (PAD) that creep up on you gradually until they can be ignored no longer. The entry point into the health care system for treatment of chronic vascular diseases is not as straight a path as, say, myocardial infarction. We know this from the recently published results from Abbott’s multi-year global research initiative, Beyond Intervention. This year, Abbott delved further into understanding the challenges that arise during the earliest stages of the vascular patient journey – from screening and symptom detection/ recognition to specialist referral. Abbott surveyed over 1,800 stakeholders across 13 countries from April to June 2021, including 1,289 vascular disease patients, 408 physicians, and 173 healthcare administrators.
The study uncovered many variations in how people experience the journey to diagnosis, treatment, and recovery, driven by factors such as disease state, socioeconomic status, and inter-physician communication. In particular, the research confirmed that patients with peripheral artery disease (PAD) face an even greater number of challenges to early and accurate diagnosis than patients with coronary artery disease (CAD) – as do women and patients from underserved communities.
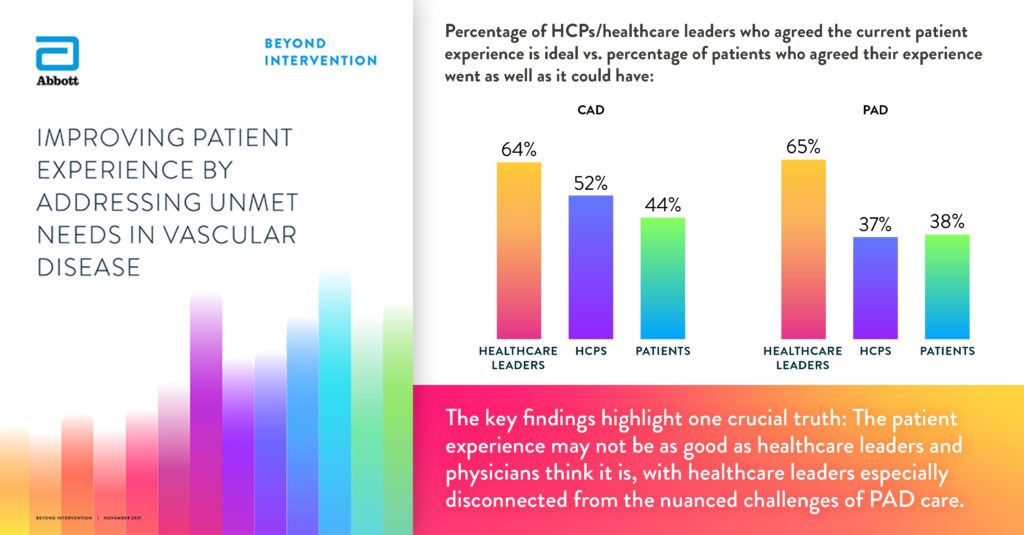
It was clear from the research the patient experience is not as positive as healthcare administrators think it is. The perspectives of Canadian patients and physicians are aligned with the global data – 46 per cent of patients feel their experience went as well as it could have, compared to a 40 per cent global average. 50 per cent of physicians feel the patient experience is ideal, compared to a 46 per cent global average. However, 90 per cent of Canadian healthcare administrators feel the experience is ideal, whereas the global average is only 64 per cent.
If the future of vascular care is going to change the current patient experience for the better, the research suggests that setting industry-wide standards in diagnostic technologies, including tools, processes and training, can optimize the patient experience. This will enable physicians to make faster, more accurate diagnoses and referrals – one patient at a time.
While access to or lack of technology is not sited as a key barrier to an early an accurate diagnosis for patients in Canada, physicians, healthcare administrators and patients have a difference of opinion about which technology solutions they think would be most helpful in diagnosing vascular diseases before they become an emergency. Patients ranked state of the art imaging as their top choice. For physicians, wearables and implantable digital health trackers ranked as the top technologies of choice. And finally, healthcare administrators ranked connected home care services, telemedicine, and remote adherence monitoring as their top choices.
The desire for more cohesive, individualized and efficient vascular care continues to surface in Abbott’s research. Achieving this ideal patient experience is possible – the technologies designed to automatically detect blockages in arteries and help physicians make better treatment decisions do exist, as do the technologies that educate and monitor patients about their symptoms. While there is no simple solution to the challenges of improving the patient experience, we continue to make progress on the future of vascular care, one patient at a time.
Learn more: cardiovascular.abbott/beyondintervention


![AV1328-164-BeyondIntDftSocGrph-LinkedIn@3x[2]](https://hospitalnews.com/wp-content/uploads/2021/12/AV1328-164-BeyondIntDftSocGrph-LinkedIn@3x2-scaled-e1639757368950-696x606.jpg)