By Julie Bortolotti
Data drives better decisions.
Throughout the pandemic, the availability of credible and timely data has been at the core of many conversations and decisions related to COVID-19. The Canadian Institute for Health Information (CIHI) has been a key partner in the response — collecting and providing data, and supporting all levels of government through modelling, standards, resources, analysis, and expertise.
Although COVID-19 has undoubtedly disrupted our health systems, many of the challenges were known well before the pandemic. The health care workforce, the sustainability of health spending, and Canada’s aging population continue to be drivers that test our systems.
Below are a few highlights of what we’ve learned about COVID-19 over the past year.
There were considerably fewer emergency department (ED) visits during the first wave
- Visits to EDs across Canada declined by almost 25,000 a day during the first wave of the pandemic — about half the usual number of patients.
- Although ED activity declined during the first wave, people with unplanned health concerns like cardiac events and trauma still received care.
- People waited less time to see a physician in the ED because of the decreased number of people coming in for care.
Hospital stays for substance use harms increased
- During the first months of the pandemic there were 81,000 hospital stays for harm caused by substances like alcohol, opioids, stimulants and cannabis — an increase of about 4,000 compared with the same period in 2019.
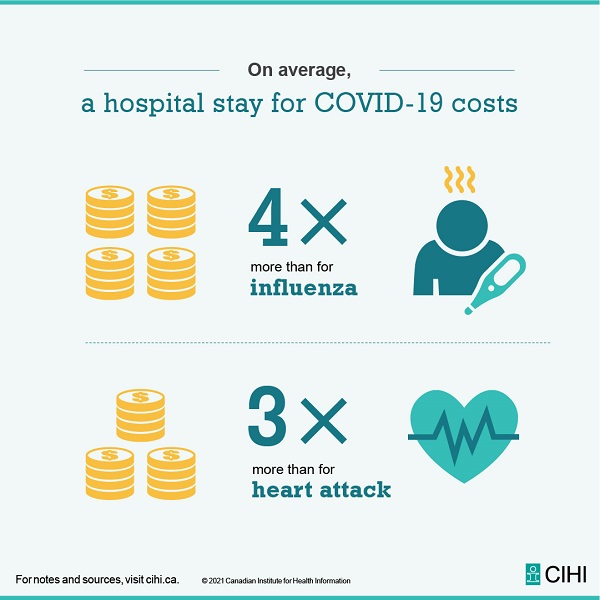
A COVID-19 hospitalization costs about three times more than a stay for a heart attack
- The estimated average cost of a hospital stay for COVID-19 is over $23,000, which is about three times more than a stay for heart attack ($7,000).
- From January 2020 to March 2021, there were over 42,240 hospital stays in Canada (excluding Quebec) for patients with COVID-19.
There were longer wait times for some priority procedures
- Cancelled and delayed procedures because of the pandemic led to longer wait times for joint replacements and cataract surgeries in 2020.
- About half of Canadians who needed a procedure didn’t receive it within recommended time frames. However, for urgent procedures like radiation therapy and hip fracture repair, most people continued to receive care within benchmark time frames.
Our health workforce experienced many effects of the pandemic
- Canada’s supply of health care workers increased as nearly 6,000 nurses, pharmacists, physiotherapists and occupational therapists returned to their practices to help respond to the pandemic, as well as new entrants to the professions.
- Despite the increase in supply and the ability to call on health care workers who weren’t working in profession-specific roles, infections and exposure to the virus among health care workers contributed to staff shortages.
- To reduce the spread of COVID-19, many health care professionals transitioned to virtual care, with about 83% of physicians providing at least one virtual care service (in selected provinces).
COVID-19 costs are expected to reach $23 billion in 2021
- Canada is expected to spend a new record of $308 billion on health care in 2021.
- Total health spending is expected to have increased by more than 12% between 2019 and 2020, a rate of increase we haven’t seen in more than 30 years.
- Hospitals, physicians and drugs continue to make up the largest areas of spending.
- A new spending category COVID-19 Response Funding will make up about 7% (approximately $23 billion) of total health spending.
As we continue to navigate the pandemic and receive more timely data, we’ll learn more about COVID-19’s effect on health systems across the country.
For more information, visit the COVID-19 resources web page for key reports and resources.
Julie Bortolotti is a Communication Specialist, Canadian Institute for Health Information.