By Kelly O’Brien
More than three million Canadians have diabetes, a number that has nearly doubled since 2002 and continues to grow. They have tools to manage their glucose levels, but not to manage foot wounds that often lead to infection and amputation.
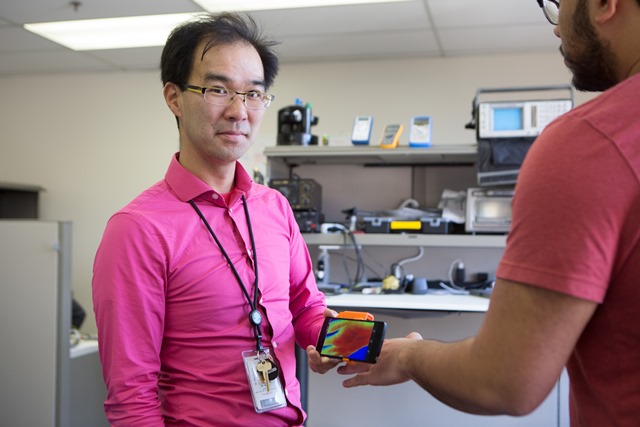
MIMOSA (Multispectral Mobile Tissue Assessment Device) is an early-detection tool developed by Dr. Karen Cross, a surgeon-scientist at St. Michael’s Hospital, and Dr. General Leung, a magnetic resonance physicist at St. Michael’s. The device detects poor blood circulation in the feet, which can lead to diabetic foot ulcers, by photographing the skin with near-infrared light.
“It’s just beyond the range of human vision , so it’s safe, but also it has deep penetration into the skin, so it’s going to get below that top layer,” says Dr. Cross. “It can see things that we can’t.”
Dr. Cross likened the light MIMOSA uses to the technology used to discover that Leonardo da Vinci was the artist behind The Adoration of the Magi, the painting most often attributed to Filippino Lippi. The light allowed art historians to view the different layers of the painting without damaging it.
“We’re doing the same thing,” explains Dr. Cross. “Before, to see how much hemoglobin you have, you’ve got to take blood. You’re damaging something by putting a needle in there. We can actually do it without damaging anything.”
Between 15 and 25 per cent of people with diabetes will have a foot ulcer at some point. These ulcers often become infected and as a result, diabetics are 23 times more likely than the general population to have a lower limb amputation. The technology MIMOSA uses to monitor wounds was originally developed as an early detector and triage tool for determining burn depth. But what has changed is the size of the tool.
“Because of the way the technology’s changed, and because we have so much computing power in our pockets with our cell phones, we’re able to shrink it down,” says Dr. Leung. “So now it’s evolved from being ten or twelve feet tall to being a little clip-on device.”
The device is designed to work for all diabetics, no matter their age or level of mobility.
“This is something you could put on a selfie stick and put it down below and take a picture,” says Dr. Cross.
The team has already seen success using MIMOSA to monitor wound development in a recently completed pilot study, and will soon begin work on a two-year, multicentre randomized controlled trial.
Evidence has also shown prevention strategies such as MIMOSA can result in a 20 to 40 per cent reduction in treatment costs.
“Diabetes is a global tsunami,” she says. “More than 300 million people worldwide have diabetes, and that number is only growing. So something that can be made quite simply and can reduce those costs is an easy sell. That’s what we want to do.”
Kelly O’Brien works in communications at St. Michael’s Hospital.

