By Melissa Stark
Until recently, like many other hospitals across Canada, the New Brunswick Heart Centre (NBHC) faced ongoing challenges with surgical wait times. Despite the implementation of various initiatives aimed at addressing the issue, patients still waited too long for cardiovascular surgery and the number of patients on the wait lists continued to grow.
Now that has started to change and the hospital is making substantial progress in delivering quality care in a more timely manner, thanks to a collaboration with the regional health authority, Horizon Health Network, and Medtronic Integrated Health Solutions (IHS), a division of the global medical device manufacturer Medtronic plc, which partners with health care providers to help them enhance access, cost and care.
NBHC is a provincial centre of excellence and the only provider of adult tertiary cardiac care for New Brunswick and Prince Edward Island. Located within the Saint John Regional Hospital (SJRH), it delivers a wide range of cardiac care and support services to more than 17,000 patients annually, and is responsible for meeting an ever-growing demand for advanced care within its existing budget.
Under a five-year partnership that began in May 2016, Horizon and Medtronic IHS are working together to improve access to five clinical services provided at NBHC. They identified cardiovascular surgery wait times as the most pressing need and the focus of the first phase of the collaboration.
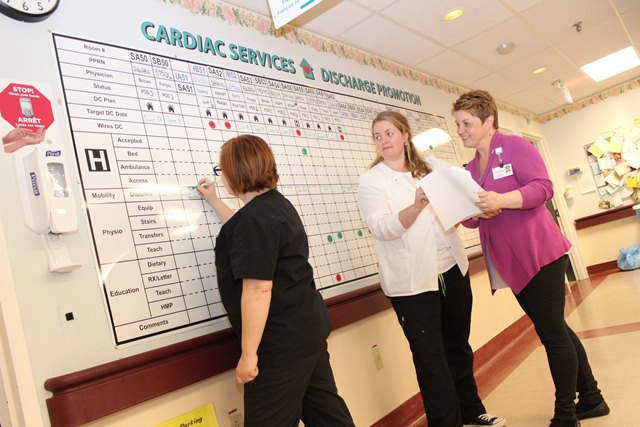
More than 800 cardiovascular surgeries are performed at NBHC each year. Meeting the Canadian Cardiovascular Society’s guidelines for recommended maximum wait times has been an ongoing challenge. The new partnership aimed to address the issue by applying Lean Six Sigma principles of continuous improvement to optimize the processes involved and in order to improve the patient experience, clinical productivity and quality of care.
Many people were involved in the initiative, including teams from Horizon and Medtronic IHS as well as senior administrative and clinical leaders, physicians and staff from NBHC and SJRH. Under the direction of a steering committee, a core team oversaw the activities of individual project teams composed of more than 50 subject matter experts who worked on the design and execution of the various aspects of the project.
The planning stage included a review of current programs and operations at NBHC, interviews with key stakeholders and data analysis. One Kaizen (continuous improvement) team focused on optimizing surgical processes, all the way from the initial decision to operate to the completion of the procedure, while another concentrated on all activities related to patient flow before and after surgery.
The planning culminated in a four-day Kaizen workshop where the teams defined and analyzed their findings and identified areas for improvement. For example, one key problem area was capacity in the intensive care unit (ICU), which frequently led to operating room (OR) cancellations. The teams also prioritized solutions, identified potential risks and developed detailed action plans with the owners of each process. In addition, they linked the solutions they developed to overall business goals and objectives.
Four key areas of focus emerged from the workshop: increasing OR capacity, reducing OR cancellations, reducing average length of stay (ALOS) in the ICU, and reducing ALOS in the step down unit.
Then the execution of the plans began. Progress was monitored regularly and challenges were reviewed and managed. A weekly dashboard reported key performance indicators (KPIs), providing visibility for individual aspects of the project as well as timely feedback on overall effectiveness.
The results of this initial phase of the project have been impressive. Within the first six months after the Kaizen workshop, OR capacity was increased by 14 per cent, median wait times were reduced by 44% from 118 to 66 days, and 90th percentile wait times fell by 31 per cent from 283 to 195 days. These trends are expected to continue as time goes on. Significant improvements in the number of cases waiting in the queue has yet to be realized, but are expected.
Through increasing NBHC’s capacity and efficiency in handling patients, the project has improved the quality of care, provided insights that will be invaluable in controlling costs in the future, and further promoted a culture of continuous improvement within the organization.
This initiative has demonstrated that innovative partnerships with health organizations, healthcare professionals and industry can lead to better care for patients, while improving efficiencies and ensuring sustainability of health care services.
Melissa Stark is a Process Improvement Facilitator at Horizon Health Network.

