By Anne MacLaurin, Virginia Flintoft, Wayne Miller and Alex Titeu
All healthcare leaders, providers, patients, and the public should wrestle with a fundamental question: How safe is our care? The typical approach has been to measure harm as an indicator of safety, implying that the absence of harm, is equivalent to the presence of safety. But, are we safe, or just lucky? Jim Reinertsen, MD, a past CEO of complex health systems and a leader in healthcare improvement, suggests that past harm does not say how safe you are; rather it says how lucky you have been. After learning about the Measurement and Monitoring of Safety (MMS) Framework, Reinertsen found the answer to his question, “Are we safe or just lucky?”
“The Measurement and Monitoring of Safety Framework challenges our assumptions in terms of patient safety,” says Virginia Flintoft, Senior Project Manager, Canadian Patient Safety Institute. “The Framework helps to shift our thinking away from what has happened in the past, to a new lens and language that moves you from the absence of harm to the presence of safety.”
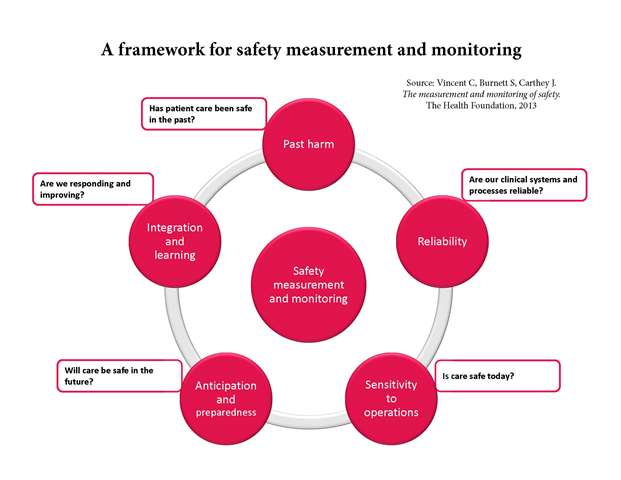
Professor Charles Vincent, Professor of Psychology at Oxford University, advocates that assessing safety is not the same as counting harm. As the first author of the Measurement and Monitoring of Safety framework, he believe it is critical for us to ask five questions, each related to a specific dimension of safety, in order to determine whether an organization is safe. This approach is one often used by industry that looks at leading and lagging indicators, and relies on soft intelligence. A holistic view of safety prompts leaders and providers to be inquisitive and empowers everyone to take a proactive role in safety.
The five critical questions are:
- Has patient care been safe in the past? Systematically reviewing existing measurement and monitoring of past harm can increase your understanding and help you to respond appropriately to harm when it occurs.
- Are our clinical systems and processes reliable? This dimension gauges the probability that a task, process, intervention or pathway will be carried out or followed as specified.
- Is care safe today? Sensitivity to operations focuses on the day-to-day, hour-by-hour and even minute-by-minute management of safety, bringing together a mix of intelligence to help staff, clinicians, managers and leaders assess and act upon safety in real time.
- Will care be safe in the future? By focusing on the identification of possible sources of future harm, you can work to become more resilient to them. Don’t wait for things to go wrong before trying to improve safety.
- Are we responding and improving? The development of systems to promote a cycle of learning and sharing from safety incidents, multiple sources of safety intelligence and insights developed through the other domains. Integration and learning is the glue that holds a rounded safety picture together.
“The Framework changes the nature of the conversation to being more mindful and forward-thinking,” says Wayne Miller, Senior Project Manager, Canadian Patient Safety Institute and MMS coach.
In 2017, the Canadian Patient Safety Institute launched a measurement and monitoring of safety demonstration project, led by Dr. Ross Baker at the University of Toronto. An 18-month Safety Improvement Project was subsequently launched in 2018, to support healthcare teams in rewiring their thinking on patient safety and to work within their organizations to foster and promote this new approach to safety.
The coaches supporting the MMS collaboratives have learned that this expanded view, helps to provide a shared and consistent understanding of safety. It empowers everyone to take a proactive role and promotes a culture of collective responsibility for safety. MMS promotes the importance of the contribution that patients and carers make to safer care. Most importantly, it reinforces the message that safety is more than counting harm.
“It is exciting to see the transformation within the teams and their understanding and focus on patient safety,” says Anne MacLaurin, Senior Program Manager, Canadian Patient Safety Institute and MMS coach.
Danielle Bellamy, Director of Continuing Care, Yorkton & District Nursing Home (Saskatchewan Health Authority) participated in the MMS collaborative. She says that the value of this work is how it empowers team members to focus on the presence of safety.
“We often speak about how safety is everyone’s responsibility, but team members have historically told us that they don’t feel they have the tools to take action,” says Bellamy. “This Framework has given us the opportunity to co-create a tool to empower our frontline team to not only identify the potential for harm, but to work towards reducing or eliminating the harm. As a result, we are witnessing a shift in the culture of safety within our care home, and providing a safer environment for both our residents and team.”
Crystal Browne, Director Clinical Operations, Alberta Health Services – Area 4 (North Zone) says, “I think the biggest takeaway I have gained from this learning collaborative is that safety is not a ‘project’ with a defined beginning, middle and end. It’s an ethos of constant inquiry at all levels of the organization as we try to answer the questions of is care safe today? and will it be safe tomorrow?”
Virginia Flintoft, Anne MacLaurin, Wayne Miller and Alex Titeu are coaching the 11 teams from across the country participating in the MMS Safety Improvement Project, helping them to implement this new approach to measuring and monitoring of safety. For more information, visit www.patientsafetyinstitute.ca