
It was around lunchtime and the Geriatric and Medical Rehabilitation unit at Providence was bustling. Jamar Stanton, a patient experience coordinator, had stepped into a patient room to ask a patient about his experience at the hospital when the patient let Stanton know that they were hungry. The lunch being served that day wasn’t to their taste, but the patient’s family had prepared them meals for such occasions.
Noticing how busy the unit was, Stanton took it upon himself to find the patient’s food in the unit fridge and heat it up for them.
“They were able to eat it and really enjoyed it,” recounts Stanton. “I was happy to do that myself and the patient was very grateful and appreciative of that as well.”
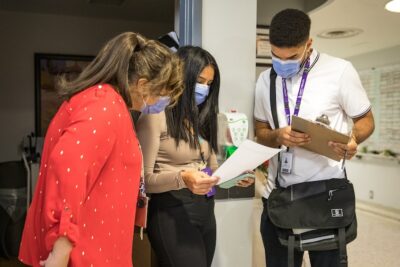
This happened during an interview Stanton was doing as part of Unity Health’s Real-time Feedback program. Stanton and his counterparts at St. Joseph’s Health Centre and St. Michael’s Hospital go to various units once a month to interview patients, learn about their care experience and get feedback that is delivered back to the units on the very same day.
“Our goal is to give patients a voice, to let them be heard and to strive for improvement,” says Stanton. “A lot of patients are glad to be given that opportunity, even if it’s just to say you guys are doing a great job.”
Stanton has been doing Real-time Feedback program interviews since February 2023. He can recount many instances where he has directly contributed to a better experience for a patient, or where he has passed along feedback that likely wouldn’t be surfaced otherwise.
“We definitely have a positive impact on people’s care,” says Stanton, speaking of himself and his fellow patient experience coordinators.
“Our goal is to give patients a voice, to let them be heard and to strive for improvement.”
Results from the Real-time Feedback program have been overwhelmingly good, with patients responding positively to 94 per cent of all questions in the interviews.
Caroline Monteiro, patient care manager, and Tiffany Nicoloff, clinical operations lead, work together on the Orthopedic and Amputee unit at Providence. Both were part of the working group that helped bring the Real-time Feedback program to life.
“It provides some validation to the staff that they are doing a good job, especially given how busy it’s gotten throughout the pandemic,” says Nicoloff.
“It shows the staff that what they’re doing is meaningful to patients,” adds Monteiro. “And for that small percentage of patients where we didn’t meet their expectations, it opens up an opportunity for quality improvement.”
The Real-time Feedback program is live on ten different units at Unity Health with plans to spread the program even further across the organization.
Measuring to improve
The Real-time Feedback program is one part of a broader Care Experience Measurement Framework. Recognizing an opportunity to gather more comprehensive data on the care experience at Unity Health, the Patient Experience and Engagement team began updating the surveys and surveying methods across the network in 2020.
Patrick Soo, a project manager who has been leading much of this work, highlights the importance of partnering with patients and families.
“We have had patient and family partners involved from the beginning to help co-develop all of the surveys,” says Soo. “Also foundational to all of our work is having all the survey and interview questions aligned to Unity Health’s Care Experience Charter.”
The Care Experience Charter is Unity Health’s road map to creating excellent care experiences together with patients and residents at the network. It was co-created by Unity Health and its patient, resident and family councils.
Currently, the Patient Experience and Engagement team coordinates surveys for inpatients at all three sites, where patients receive a call after their discharge. They also do surveys for outpatients at the three sites and Emergency Department (ED) patients at St. Joseph’s and St. Michael’s, where patients receive a call or email after their visit.
In October, they began in-person interviews with residents of the Houses of Providence long-term care home.
Unity Health response rates for these surveys are quite good – 50 per cent for inpatients, 40 per cent for outpatients and 30 per cent for ED patients. These response rates are up 20 per cent or more when compared to the network’s previous survey vendor.
Adding the Real-time Feedback program has helped to give units more insight into the patient experience at different points in the care journey and provides an opportunity to course correct a patient’s experience before they leave. This is an opportunity Unity Health has not had in the past.
“The real-time patient data allows us to capture patients throughout the spectrum of their journey, whether at admission, they’re midway or they’re close to discharge,” says Monteiro.
The data for each clinical area is summarized and reported back to leaders so they can identify issues, create solutions and monitor their progress.
Creating more equitable care
Unity Health is also taking a thoughtful approach to collecting data about who its patients are – such as how they identify and their education and income levels – as part of the surveys for inpatients and outpatients that are completed after their hospital stay or visit. These additional questions were developed in partnership with Unity Health’s Office of Anti-Racism, Equity and Social Accountability and in alignment with partners at Ontario Health.
The goal is to understand what the experience is like for specific groups of patients and identify opportunities for improvement that might be missed if the organization only looked at the data as a whole.
“It’s the whole tenet for our vision – The best care experiences. Created together,” says Soo. “We don’t know if we’re creating the best care experience for everyone unless we know who they are. This is our first step to actualize on that.”
This work is setting Unity Health apart as a leader in the field of patient experience measurement in Canada. They have even run a session for their counterparts in the field, hosted by the Ontario Health Association.
For Soo, it all comes back to the impact that this work has on patients, residents and their families.
“During post-discharge survey phone calls for inpatients some people will say, ‘Oh, I remember speaking with someone on the floor and then, after they left, the care team came and talked with me and everything got better,’” describes Soo. “Being able to contribute to a better experience for the patients is really a rewarding experience to have.”

