By Melicent Lavers-Sailly
A common perception that minimally invasive surgery to repair aortic stenosis is more expensive for hospitals than open heart surgery may be painting an incomplete and inaccurate picture, says a recently released Canadian research paper.
The study, Breaking Down the Silos: Transcatheter Aortic Valve Implant Versus Open Heart Surgery, conducted a budget impact analysis of therapeutic alternatives for the treatment of high-risk severe symptomatic aortic stenosis patients comparing minimally invasive Transcatheter Aortic Valve Implant (TAVI) to Surgical Aortic Valve Replacement (SAVR).
It found the overall cost of a hospital treating an aortic stenosis patient over the course of a fiscal year is marginally less when they receive TAVI because patients are generally required to spend less time in hospital and experience fewer adverse events – like life-threatening bleeding, atrial fibrillation, stroke and cardiac arrest – with the minimally invasive procedure than when they undergo open heart surgery.
“My findings indicate that TAVI is more expensive up front for the procedure itself, but it becomes slightly less expensive than open heart surgery when you consider the patient’s healthcare a year out,” says study author Hamid Sadri, Director of Health Outcomes, Research and Technology at Medtronic. “Hospitals may benefit more if they look at the cost of therapy over one year rather than the common practice of going procedure by procedure.”
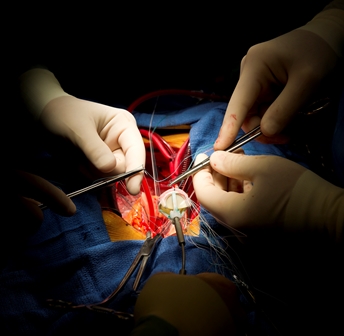
Surgical aortic valve replacement, the conventional treatment for high-risk aortic stenosis, is an open-heart procedure in which the aortic valve is surgically replaced. TAVI is a minimally invasive alternative in which a bio-prosthetic valve is implanted into the patient’s heart via a catheter inserted in their groin.
“While TAVI was initially reserved primarily for extreme-risk patients when it was first introduced a decade ago, its use has gradually been extended to patients in lower risk categories (high-risk) at many hospitals,” adds Caroline Merineau, Senior Clinical Specialist at Medtronic.
Sadri’s research examined the total cost of treating a hypothetical cohort of 100 high-risk patients with aortic stenosis, including the surgical procedure itself and the subsequent management of potential adverse events and follow-up visits over the course of a year.
He determined the average per-patient cost of performing a TAVI procedure ($52,576) is slightly more expensive than SAVR ($48,578). However, the average cost of managing adverse events in the first year after the procedure is more expensive for patients undergoing SAVR ($17,718) than TAVI ($11,754).
As a result, Sadri pegged the total cost of care in the first year for a patient undergoing a TAVI procedure at $64,330, a cost savings of $1,996 compared to SAVR, which had a total cost of $66,296.
While the savings per patient are marginal when you look at them individually, Sadri said his research has broader implications for hospitals when considering overall patient caseloads and optimizing healthcare resources.
Consideration should also be given to patient preference, he said, noting that a number of studies have demonstrated patients would rather opt for minimally invasive procedures that require a shorter hospital stay, when given the choice.
At a time when hospitals are being challenged to ensure they have capacity to deal with the ongoing COVID-19 pandemic, minimally invasive procedures, such as TAVI, can play an important role in freeing up bed capacity, adds Merineau.
“By itself one procedure may not provide substantial benefit to the hospital or to the healthcare system. But imagine 100 different procedures — if you replicate this format for multiple technologies and multiple procedures, the sum of all the savings, could be very substantial to the system,” Sadri said.
But in order to reap these types of benefits, hospital administrators would have to be willing to re-examine how they traditionally allocate budgets and deliver patient care.
“The system has created these arbitrary silos within hospitals. People tend to look narrowly at their own budgets or the cost to their department, compared to the whole cost to the hospital or the health care system,” Sadri said.
He believes hospitals may be able to realize savings while providing improved experiences for patients and hospital staff at the same time, if they were to allocate budgets based on the total cost of treating patients over the course of a fiscal year, building in the flexibility for professional judgements by clinicians, rather than making per-procedure budget allocations.
“The patient flow should dictate where the money goes, not individual departments or segments in a healthcare system,” he said. “If I go to hospital, the hospital ideally should provide me the best procedure available based on clinical judgement and clinical guidelines and provide me as a patient the best experience I can get.”
You can find a full version of Breaking Down the Silos: Transcatheter Aortic Valve Implant Versus Open Heart Surgery at journals.sagepub.com
Melicent Lavers-Sailly leads Communications for Medtronic Canada.