With the recent rise in cases of monkeypox virus, clinicians may need guidance for diagnosing and treating the virus, which is new to Canada. An article published in CMAJ (Canadian Medical Association Journal) summarizes five things to know about the virus, which is endemic to West and Central Africa.
- Monkeypox is a viral infection with person-to-person transmission through direct and close contact during the infectious stages. Airborne transmission is thought to be less common.
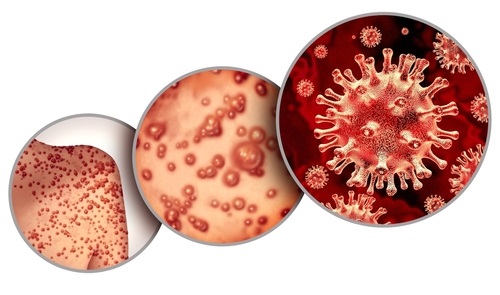
- A rash with distinct skin lesions is typically preceded by symptoms such as fever, aches and swollen lymph nodes, but not always. Clinicians should also consider syphilis, chancroid, varicella zoster, herpes simplex, hand-foot-and-mouth disease, mulloscum contagiousum, and cryptococcus. Patients are likely to be infectious from the start of symptoms until all scabs have resolved.
- Health care providers should follow airborne, droplet and contact precautions and notify public health authorities when testing for monkeypox, including for sample collection. Diagnosis is made with real-time polymerase chain reaction (PCR) testing. Consultation with an infectious disease specialist or microbiologist is advised to support clinical assessment.
- Most patients with monkeypox can be managed as outpatients.
- Smallpox vaccination is effective for monkeypox, and vaccination of high-risk contacts (ring vaccination) and contact tracing may help contain spread. People with previous vaccination against smallpox (e.g., many born before 1970) have some cross-protective immunity to monkeypox.