New approach for early cancer treatment was shown to significantly reduce the risk of advanced neuroendocrine tumour progression and death by 72 per cent in otherwise challenging areas to treat.
“This is a game changer in the practice of not only the treatment of higher Grade 2 and 3 neuroendocrine tumours of the gastrointestinal tract, but for cancer treatment broadly,” says Dr. Simron Singh, global principal investigator of the trial, and medical oncologist, affiliate scientist at Sunnybrook Research Institute (SRI) and cofounder of the Susan Leslie Clinic for Neuroendocrine Tumours at Sunnybrook’s Odette Cancer Centre.
Presented at the 2024 American Society of Clinical Oncology (ASCO) Gastrointestinal (GI) Cancers Symposium, an overview of the results from the NETTER-2 Phase III multi-centre international clinical trial provided evidence for the first time that radioligland therapy (RLT) – when applied in the early stages after a patient’s diagnosis – significantly and safely slowed down the progression of neuroendocrine tumour growth, extending the average time of “progression-free survival” from approximately 8.5 months to 22.8 months. This is the first trial to show efficacy of first-line RLT in any cancer.
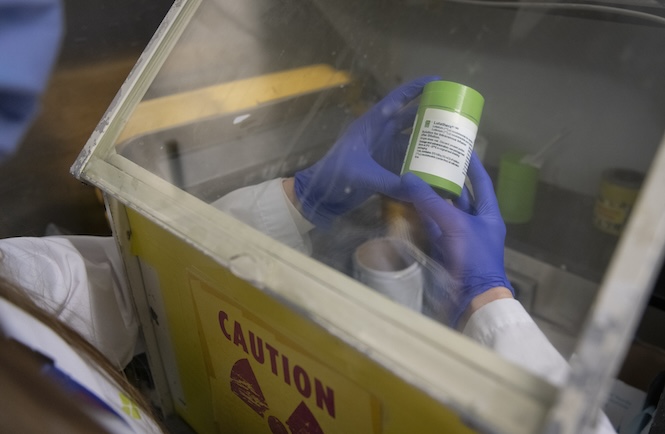
RLT – a more precise form of radiation therapy being used and researched in the treatment of some cancers – involves injecting radioactive isotopes through an IV (in this case, with the drug known as Lutathera) in order to target cancer cell receptors, and deliver more targeted and precise radiation to kill cancer cells.
This study evaluated the use of RLT earlier as a first-line (or “up front”) treatment for patients newly diagnosed with grade 2 or 3 advanced gastrointestinal neuroendocrine tumours. Although neuroendocrine cancer is uncommon, its incidence is rising rapidly and few treatments exist for these patients as this kind of cancer is resistant to most treatments; making it challenging to treat.
“The results confirm the clinical benefit of earlier use of RLT for newly-diagnosed patients with these types of aggressive and life-threatening tumours,” says Dr. Singh, also an associate professor of medicine at the Temerty Faculty of Medicine at the University of Toronto. “This is the next step in personalized targeted cancer therapy for patients, focused on more effectively killing cancer cells, while limiting the damage to surrounding healthy tissues.”
Further investigations of RLT as a therapeutic option are ongoing to evaluate overall survival and long-term safety, which will better define next steps for this change to practice in cancer treatment world-wide.
The multi-site trial included investigators and participants from Canada, France, Germany, Italy, Netherlands, South Korea, Spain, UK and USA.
World leaders in the care of neuroendocrine tumours and research, the multidisciplinary Susan Leslie Clinic for Neuroendocrine Tumours at Sunnybrook’s Odette Cancer Centre is the only one of its kind in Canada. With a team of surgical oncologists, medical oncologists, radiation oncologists, nuclear medicine physicians, interventional radiologists, dedicated pathologists, and geneticists under one roof, their integrated care model is improving outcomes for patients with neuroendocrine tumours, as it studies care delivery, trials new therapies, and leads expert consensus.

