By Donna Harris
It’s only May, and yet 2020 is already a year for the history books. For hospitals, the past few months have required heightened responsiveness and careful planning in the face of a virtually unprecedented global pandemic.
As the potentially devastating impact of COVID-19 became clear earlier this year, William Osler Health System (Osler)’s palliative care team implemented a proactive, multi-pronged plan to respond to the pending crisis. “We expected that as the number of people with COVID-19 increased, many of those individuals would require palliative care and we began preparing to compassionately serve the needs of COVID-19 patients, in addition to the other patients with palliative care needs who would require care throughout the pandemic and beyond,” says Dr. Martin Chasen, Osler’s Medical Director of Palliative and Supportive Care.
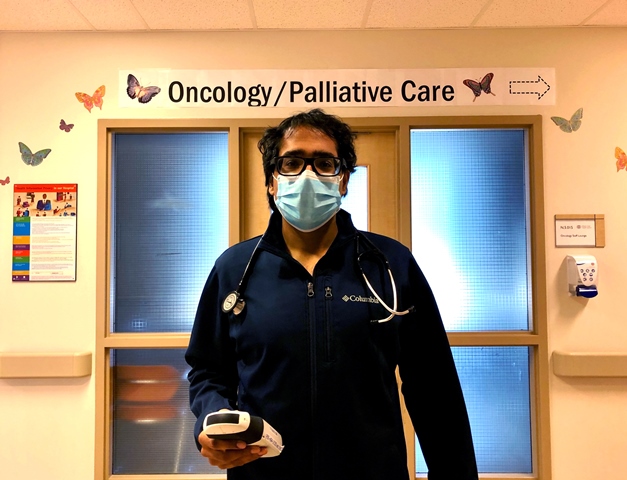
Dr. Amit Arya, a palliative care physician at Osler, agrees a proactive approach can ensure the needs of patients are met.
Recently, Dr. Arya was the lead author of Pandemic Palliative Care: Beyond Ventilators and Saving Lives in the Canadian Medical Association Journal (CMAJ). The article details eight critical elements for providing palliative care during COVID-19, including supplies, staffing, systems and communication – all components that have been taken into consideration in Osler’s planning. “This comprehensive approach is necessary to help ensure patients continue to receive high-quality care,” says Dr. Arya.
Supporting care in the community
While Osler’s palliative care team has always worked closely with its health care partners, collaboration took on an enhanced focus in light of the new virus.
“It has never been more important to ensure that people receive the care they need in the most appropriate setting throughout their health care journey,” says Dr. Chasen. “While we certainly want people who need emergency care to access the Emergency Department (ED), we also don’t want them exposed to the possibility of a hospital-acquired infection. In many cases, unless patients are truly in need of emergency care, they are better served to receive treatment outside of the ED, in the community.”
To facilitate this, Osler’s palliative care team contacted primary care and home care providers to relay the support Osler could provide, educate them about how to provide basic end-of-life care themselves, and reassure them that the palliative care team is available to support them 24/7.

In addition, the team consulted with long-term care homes caring for COVID-positive residents, some of whom also require end-of-life care, and began working with long-term care staff to reduce unnecessary resident transfers to hospital. Three Osler palliative care staff have been seconded to support palliative care needs in long-term care homes virtually and are available on-call to provide in-person consults at the homes. That is in addition to visiting and treating COVID-19 patients directly in other areas of the community.
Providing virtual care options
Leveraging technology to provide care offers enhanced protection for patients and families, as well as health care providers who risk spreading COVID-19 further as they travel between facilities. And technology is helping Osler address another challenge: families unable to visit loved ones during their end-of-life journey.
“Visiting policies have become necessarily much more restrictive at all Osler sites,” says Dr. Arya. “We recognize that these measures, although necessary, are extremely difficult for many families and we are arranging virtual family conferencing whenever possible.”
Patients with palliative care needs are using Osler’s award-winning RELIEF app to virtually self-report their symptoms to clinical teams on a daily basis. Nurses monitor patient data in real time and intervene if symptoms become more troublesome. Use of the app has also been shown to prevent unnecessary hospitalizations and visits to the ED, as well as reduce distress. It allows health professionals to closely monitor the symptoms of both palliative and COVID-positive patients – and provide care for more people.
Increasing capacity to provide more care
A teaching site for the University of Toronto and McMaster University medical students, Osler has partnered with both schools to formulate best standards of practice for delivering care during the COVID-19 crisis. When complete, the standards will be available to health care organizations around the world – a contribution with potentially global impact.
To help meet the rising demand for care locally, Osler invited physicians and surgeons who specialize in other fields and are not currently practicing palliative care to participate in focused palliative care training to support the growing needs of COVID-19 patients. The goal is to increase palliative care capacity within the community by two thirds, and care for more people.

