
In 2015, Sunnybrook Research Institute (SRI) scientists and clinicians performed a world-first: They successfully and non-invasively opened the blood-brain barrier to deliver chemotherapy into the brain tumour of a patient using MRI-guided focused ultrasound. The procedure – which was part of a clinical trial – hailed a new frontier in focused ultrasound that could transform the landscape of brain medicine.
Nearly 10 years later, the same group of researchers is once again approaching a new breakthrough, this time with the potential to bring the technology to more patients and more clinics, and to revolutionize the treatment options for many neurological and brain diseases.
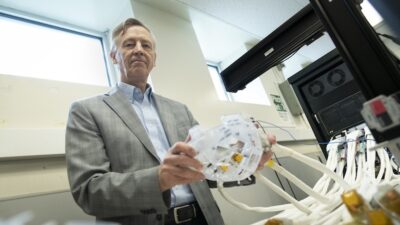
The team, led by Dr. Kullervo Hynynen, vice president of research and innovation and senior scientist at SRI, has developed a powerful new ultrasound device specifically designed to open the blood-brain barrier to allow helpful agents – such as chemotherapy, antibodies, stem cells or gene therapy to reach the brain. However, unlike the current focused ultrasound device, the new technology operates without the need for real-time MR imaging – a costly hurdle for delivering focused ultrasound to the brain.
At Sunnybrook, focused ultrasound is most commonly used to treat essential tremor, a neurological disease that causes tremors which can severely affect a person’s quality of life. Dr. Nir Lipsman, chief of the Hurvitz Brain Sciences Program and senior scientist at SRI, explains that the technology used for this indication is called high-intensity focused ultrasound, which uses ultrasound waves to target tissue and create lesions deep within the brain, without the need for a scalpel or incisions.
The new technology in development, meanwhile, is low-intensity focused ultrasound, which Lipsman says, “is used to open the blood-brain barrier and deliver all kinds of therapeutics to the brain.”
The technology behind the low-intensity focused ultrasound is currently undergoing clinical trials at Sunnybrook’s Harquail Centre for Neuromodulation– to be housed within the new Garry Hurvitz Brain Science Centre – and has the potential to provide new treatments and therapies for brain cancers, Alzheimer’s disease, Parkinson’s disease and Amyotrophic Lateral Sclerosis (ALS).
Drs. Hynynen and Lipsman shared some of the latest developments and most promising potential of the next-generation helmet.
How could this next-generation helmet change the way focused ultrasound is used to treat brain diseases?
Lipsman: One of the conditions we are most interested in is brain cancer. Currently, the entire procedure across all of our trials is done inside the MRI for real-time imaging. There are some indications where that’s very important, but there are other indications where real-time imaging may not be as critical. The next-generation helmet means we may be able to do the procedure outside of the MRI environment, saving time and money, and making the procedure more comfortable for patients. The idea is over time to develop a safer, more streamlined, and effective procedures for accessing critical brain circuits, and that’s where the new technology will really shine.
Hynynen: Taking the procedure out of the MRI would make it a more accessible form of treatment. We would do an initial scan of the patient’s head to be able to create a rapid prototype of the helmet that is customized to the patient, and subsequent treatments could be done without real-time imaging. Being out of the MRI means no associated costs, and by bringing costs down it increases
capacity significantly.
How is the next-generation helmet different from the existing technology?
Hynynen: The current focused ultrasound technology works really well for precise single ‘dose’ treatments, like treating tremors or what you might think of as ‘surgery’ treatments. But for treating brain cancer or Alzheimer’s, which require multiple treatments, it becomes prohibitive in its current state using real-time MRI. By taking the treatment out of the MRI, we can perform any number of treatments. It’s taking it to the next level – it becomes a real treatment for things like brain cancer and Alzheimer’s.
What would a treatment visit look like for someone using this new technology?
Hynynen: The patient would get the initial MRI scan, and from that a customized helmet would be created. Then, the patient would come in for treatment, get the helmet and transducers on. We would infuse drug and infuse the microbubbles that help us open the blood-brain barrier, and with very controlled modulation we would open the blood-brain barrier to deliver the therapy. The treatment can be precisely customized for each patient to the area of the disease while the intact blood-brain barrier is protecting the rest of the brain.
Lipsman: An aspirational goal would be to do with focused ultrasound what we do in a chemotherapy clinic or a dialysis centre. It would be an outpatient procedure where patients come in, get the procedure, and leave in a more streamlined, comfortable process. Ultimately, we hope to use focused ultrasound at every stage of the brain cancer treatment journey. This can include immediately after surgery, when patients undergo chemotherapy and radiation or it might be at the time of a recurrence, and in order to enhance the effect of other treatments. The idea is to match, as much as possible, novel treatments to our patient’s specific conditions.
By Brianne Tulk
Brianne Tulk is a Communications Advisor at Sunnybrook Health Sciences Centre.

