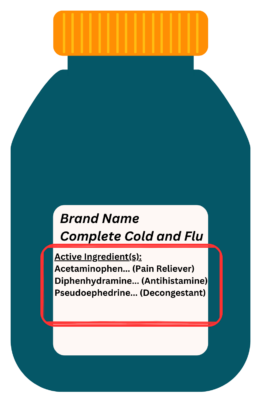
TJ, a 45-year-old male with symptoms of a common cold (sore throat, headache, runny and stuffy nose) goes to his local pharmacy, as the Acetaminophen 500 mg tablets that he has been taking at home does not seem to be strong enough to relieve his symptoms. He walks down the cough-and-cold aisle and intends to purchase a [Brand Name] Complete Cold and Flu formulation over-the-counter medication (with active ingredients: Acetaminophen, Diphenhydramine, and Pseudoephedrine) (Figure 1).
What are over-the-counter medications?
Over-the-counter (OTC) medications can be purchased without a prescription. They are usually located outside of the dispensary for self-selection by consumers/patients. Common examples include cough-and-cold medications, pain relievers, antacids, antidiarrheals, allergy medications, etc.
What are drug interactions?
A drug interaction is an interaction between two medications (including supplements like vitamins or natural health products), between a drug and food, or between a drug and a medical condition that may affect how the medication would work in the body, hence leading to potential side effects. This article will focus on the first type of drug interactions: drug-drug interactions (DDIs) with OTC medications.
Common drug interactions with OTC medications
Commonly purchased OTC products include cough-and-cold and pain relief medications. This was reflected in the above case scenario with TJ. One of the most common DDIs is duplication of therapy, that is, using two or more of the same kind/class of medications. For example, some patients may be taking OTC Ibuprofen for headache but may also be taking Naproxen (from a prescription) for another medical condition, not realizing that both medications belong to the same drug class called non-steroidal anti-inflammatory drugs (NSAIDs). If taking too much NSAIDS, it will increase the risk of side effects like ulcers, water retention, increased blood pressure, and bleeding, etc. Some OTC pain relievers contain acetylsalicylic acid (ASA) and for patients who are already on ASA or some form of blood thinners like Warfarin, they will be at an increased risk of bleeding if they take an ASA-containing OTC pain relief medication. On the other hand, many OTC products have similar active ingredients like Acetaminophen which may potentially lead to duplication of therapy if the patient is already taking another acetaminophen-containing OTC cough-and-cold products. An overdose of Acetaminophen may be associated with liver damage. Similarly, allergy medications like Diphenhydramine are commonly included in OTC cough-and-cold products as it relieves symptoms like runny nose and aids the patient in sleeping. Patients may not be aware of the drowsiness or sleepiness side effect of Diphenhydramine, and this can be of concern for patients who are concurrently taking other medications that can increase drowsiness (e.g., antidepressants/anti-anxiety medications, opioids, anti-seizure medications, etc.). Lastly, Pseudoephedrine is a common decongestant in OTC cough-and-cold products and its use is contraindicated with some types of antidepressants (e.g., monoamine oxidase inhibitors) due to a significant increase in blood pressure.
How to prevent drug interactions with OTC medications?
Consulting a pharmacist before purchasing OTC medications is the best strategy to prevent DDIs with OTC medications. Referring to our case scenario above, TJ is already taking Acetaminophen 500 mg tablets at home, and he is planning to purchase an OTC cough-and-cold product which also contains Acetaminophen. Using both products would put him at risk of Acetaminophen overdose. TJ should consult a pharmacist who would be asking him about medications that he has been taking, his symptoms, his medical conditions, his allergies, etc., before purchasing the OTC cough-and-cold product.
If consulting a healthcare professional is not feasible, then TJ can inspect the list of active ingredients of the OTC product prior to making a purchase. Most OTC products will have their indication(s) listed beside the active ingredients (Figure 1). For example, one may not be aware which active ingredient is a pain reliever when purchasing OTC cough-and-cold medication. However, when inspecting the list of active ingredients, it is mostly likely that you could identify which of them is pain reliever (e.g., Acetaminophen). If a patient is already taking another Acetaminophen-containing medication (e.g., from a prescription or another OTC), then it is best to avoid this potential duplication of therapy from an OTC product. Alternatively, there are online DDI checkers like WebMD Drugs Interaction Checker (https://www.webmd.com/interaction-checker/default.htm) where one can manually look up and check DDIs. However, it is important to note that information retrieved from these self-help online tools should not be considered as a replacement or substitute for the advice or consultation from a pharmacist or your primary healthcare professional/provider. The best strategy to prevent DDIs is to speak to your pharmacist and your healthcare
provider.
By Uroosa Abbas and Certina Ho
Uroosa Abbas is a PharmD Student at the Leslie Dan Faculty of Pharmacy, University of Toronto; and Certina Ho is an Assistant Professor at the Department of Psychiatry and Leslie Dan Faculty of Pharmacy, University of Toronto.]


