By Dale Mayerson and Karen Thompson
‘Dysphagia’ means a problem with swallowing and this can happen for many reasons. Any disease, treatment or surgery that weakens or damages the muscles and nerves used for swallowing may cause dysphagia. Common conditions that may affect swallowing include stroke, dementia and Parkinson’s disease.
Why are swallowing problems dangerous?
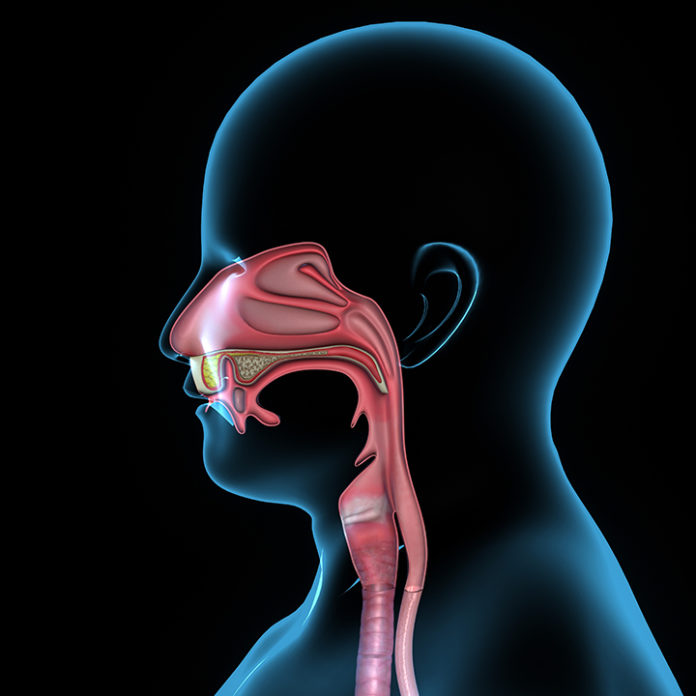
In the throat there are two tubes that are side by side. When a person has a swallowing problem there is a danger that food or drink may go into their trachea or windpipe (breathing tube) instead of their esophagus (eating tube). This can sometimes cause a chest infection or pneumonia which can be life threatening.
As well, people with difficulty swallowing sometimes don’t take in enough food or fluid. This can cause them to lose weight or become dehydrated, which can lead to other medical conditions, physical disabilities and mental confusion.
How do you know if you have a problem with swallowing?
Some people have clear signs that they are having difficulty while others show no signs.
Some common signs and symptoms may include
- Coughing or choking while eating or drinking or soon after eating or drinking
- Clearing the throat frequently
- Wet, gurgly voice after eating/drinking
- Swallowing many times for each bite
- Drooling (saliva or food)
- Trouble getting the swallow started
- Trouble clearing food from the mouth or throat after swallowing
- Chest congestion after eating or drinking
- Pain during swallow
- Unusually slow eating/ holding food in mouth
- Needing extra effort to chew or swallow
- Tiredness or shortness of breath while eating
- Watering eyes when eating
- Regurgitation
- Fever or rising body temperature
- Loss of weight due to not finishing meals
- Pneumonia or chest infections
How to Manage Dysphagia
Usually it is helpful to change the person’s food or drink consistency to make swallowing safer and easier. A swallowing assessment is useful to determine which textures can be swallowed easily and safely. It may be done in-house by a member of the healthcare team, or by a Speech Language Pathologist (SLP).
Food
When a person has swallowing problems, changes in diet texture can give more control, making it easier to swallow and reducing the risk of aspiration, which could lead to pneumonia.
Examples of different food textures include
- Pureed – foods are pureed in a blender until completely smooth (example pureed peaches)
- Minced – food is ground or finely minced and moisture is added so it is not dry (example shepherd’s pie
- Minced Meat or Soft – meat is ground or finely minced (hamburger patty)
- Hard Solids (example nuts)
Some people with swallowing difficulty may be better off when they avoid sticky foods such as peanut butter, bread, and cheese, or crumbly foods such as crackers, cookies and muffins. Often foods with two or more textures such as cold cereals with milk, and chunky soups are best avoided.
Fluids
A swallow assessment will also determine drink textures that are swallowed easily and safely. Drinks or thin liquids including water, tea, coffee, juice or soup, can be difficult to swallow because they move very quickly down the throat and may enter the breathing tube.
Drinks can be thickened to make them easier and safer to swallow, or they may be avoided by substituting moist food items. For example, a person could have pudding or yogurt instead of milk, or applesauce instead of juice.
Examples of Drink Textures include
- Pudding thick –(thick) – falls off spoon like pudding, must be eaten with a spoon
- Honey thick – (slightly thick) – runs off spoon like honey, may be taken from a glass or eaten with a spoon
- Nectar thick – Slightly thicker than water, must be taken from a glass
- Regular/thin – example water, juice
It is important to note that there has been an international initiative working towards standardizing the definitions of texture modified food and fluids used to address dysphagia. See www.IDDSI.org for more information. The new terms and textures were recently introduced and it is expected that these will be in full use within the next couple of years.
Other Strategies
Other ways to improve swallowing may be recommended including specific head positions when eating and drinking. Positioning at meal times can also improve safety and comfort when eating. Sitting in a chair with hips and knees at 90 degrees with chin slightly tucked down is the safest body position for safe swallowing. An Occupational Therapist (OT) can assist in planning for more challenging issues with body positioning while a Speech Language Pathologist (SLP) may be asked to participate in developing a plan for safe ingestion. Physicians and Nurses may identify other concerns affecting swallowing such as the effects of medications, physical limitations and other medical conditions.
Best practice would ensure Homes have a program in place that support multi-disciplinary:
- Assessment of swallowing problems
- Dysphagia care conferencing
- Care planning that is clear and easy for staff to follow
- Quarterly reviews of resident’s acceptance and success and challenges with strategies
In addition, LTC homes need to support staff and volunteers with frequent training on safe feeding techniques and to provide residents and decision-makers with information on swallowing disorders that is user friendly and easy to understand.
Tips for safe eating and swallowing
□ Reduce distractions – example turn off the television or radio
□ Eat and drink only when fully awake
□ Sit up straight in a chair or bed
□ Be sure to wear dentures, hearing aids and glasses at all meals
□ Be sure mouth is clean and clear of food particles before and after meals
□ Tuck chin slightly downward towards the chest while eating and drinking
□ Take small bites and sips
□ Make sure to swallow the first bite or sip before taking the next one. Watching for movement of the Adam’s apple/throat will help to show if the person has swallowed
□ Remain sitting up straight for 20 to 30 minutes after eating
□ Try to have a slow and relaxed dining experience
□ If coughing or choking occurs, stop eating until it has stopped
□ Tell the staff if you notice someone who is having trouble eating or drinking
Dale Mayerson, B Sc, RD, CDE, and Karen Thompson, B A Sc, RD are Registered Dietitians with extensive experience in Long-term care. They are co-authors of “Menu Planning in Long Term Care and Retirement Homes: A Comprehensive Guide” and have participated for many years on the Ontario Long Term Care Action Group, an advocacy group of Dietitians in Canada.