By Ellen Rosenberg
A blood transfusion process that once took about four hours out of a patient’s day has now been cut in half, thanks to one unit’s commitment to enhancing patient care.
On Toronto Rehab’s 8 South Multi-System Rehabilitation Inpatient Unit, located at University Centre, a team of nurses dedicated the later part of 2021 to learning how to administer blood transfusions directly on their unit.
That means patients who used to spend hours preparing to leave the unit, transport to another UHN site, receive a transfusion, travel back and settle in, can now receive the same care, from the comfort of their own bed, in a fraction of the time.
Training unit nurses to administer blood transfusions is a natural evolution for the team on 8 South, says Yolande Geba, Program Services Manager on the unit.
“It reflects Toronto Rehab’s ongoing commitment to matching patient need to scope of practice, removing barriers to admission, and enhancing patient experience,” Yolande says.
It also frees up a patient’s time to focus on reaching their rehab goals and spending time with essential care partners.
Matching scope of practice to patient need
Across all programs at Toronto Rehab, teams are caring for increasingly complex patients. It’s part of an effort to support patient flow in acute hospitals, and ensure equitable access to rehabilitation.
Individuals recovering from oncology or transplant surgery represent just two populations whose medical needs were, until recently, beyond the scope of what was delivered on-site.
“Some of our patients may require frequent blood transfusions as part of their treatment plan,” says Kristen Cunningham, an advanced practice nurse educator for the MSK and Geriatric Rehab programs.
“In the past, we’ve admitted them to our unit, coordinated their outpatient blood transfusion appointments with Princess Margaret or Toronto General Hospital, organized their transfers, helped them prepare to leave, then settle back in, upon return.”
From a resourcing perspective, the process was costly.
From a patient perspective, it was disruptive, and involved a number of teams and transitions where errors could occur.
The solution was to train nurses on 8 South to administer blood transfusions.
“Localizing all care needs in one place promotes patient-focused care,” says Daltash Dhaliwal, a clinical nurse specialist who partnered with Kristen and UHN’s Transfusion Safety Officer, Farzana Tasmin, to provide the education.
“Our nurses have the capacity to provide excellent care, and we want to continue to empower them to work to their full scope,” Daltash says.
Simulation brings education to life
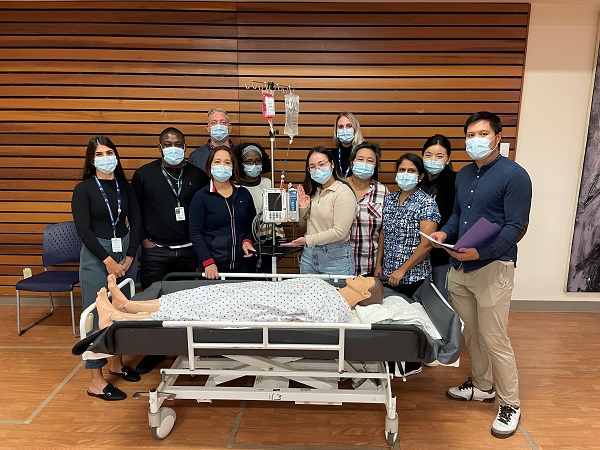
The nursing education, which took place throughout October in the auditorium at University Centre, included one hour of didactic theory, and one hour of interactive, hands-on application in a simulated lab.
From start to finish, the nurses practiced analyzing a new order, requesting blood from the lab, spiking the blood, delivering the transfusion, and monitoring the patient throughout the entire process.
“We even created a scenario where the patient had a transfusion reaction, and the team had to react and adapt, as they would in a real setting,” says Daltash.
“While nurses in rehab have experience administrating IV medications, blood transfusions are different. The policies, logistical processes and assessment requirements to perform this skill is brand new.”
Nicoleta Ciuca, a nurse on 8 South, says she and her colleagues have been looking forward to enhancing their skills, and found the education to be helpful in clarifying the process, from start to finish, and in identifying the resources they’d need.
“The theory is important,” Nicoleta says, “but we had a lot of logistical questions that the hands-on simulation helped clarify: Who is going to bring the blood from the blood bank? How are we going to get it to our patients?”
Allowing patients to focus on their rehab goals
Back on 8 South, Nicoleta says her confidence in this new area increases every day, thanks to ongoing support from Kristen and Daltash. But what really stands out for her is how it’s enhanced her patients’ experiences.
“We want patients to be focusing on their rehab goals,” she says. “Now we have some flexibility to work around their therapy appointments, meals, and practicing other activities of daily life.”
Kristen agrees, adding that, by the time they’re admitted to rehab, many patients have had a long, complicated, and sometimes stressful journey.
“To be able to come here, settle in, and not have to be shuffled back and forth between care teams, will really enhance their patient experience and propel their rehab forward,” she says.
Ellen Rosenberg is a Senior Public Affairs Advisor at University Health Network.