By Dr. Craig Earle
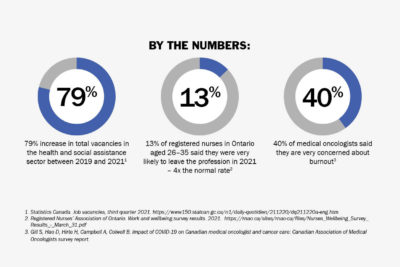
Canada’s cancer care professionals continue to do their utmost to provide excellent care through wave after wave of the COVID-19 pandemic, despite overwhelming pressures. However, the disruptions are taking their toll. Attrition and burnout are on the rise. More and more job vacancies are going unfilled.
The burden on healthcare workers is heavy, and it is contributing to delays in cancer screening, diagnosis and treatment. The implications will be felt for years to come. Canada needs a coordinated effort to boost system capacity and save lives – and it is needed now.
The Canadian Partnership Against Cancer’s recent report, The road to recovery: Cancer in the COVID-19 era, identifies actions that can be taken and innovations that are already underway in some jurisdictions to provide a path forward even as COVID-19 continues to disrupt health and cancer care.
The impact of COVID-19 on cancer
The onset of the pandemic saw the cancellation or postponement of clinical exams and procedures, leading to many cancers going undiagnosed or untreated. The impact has been dire because the longer a cancer goes undetected, the worse a person’s outcomes are likely to be: a more advanced stage at diagnosis, poorer survival rates, and greater disease-and treatment-related issues.
The effect of these delays and the rising backlog of undiagnosed cases is magnified for populations that have been underserved due to differences in access to resources, power and privilege.
The burden of disease and the magnitude of avoidable deaths are greater for cancer than other conditions, and cancer must remain a priority when allocating healthcare resources.
Key to that is a focus on healthcare human resources.
The Canadian Partnership Against Cancer’s report shows that three areas need to be addressed:
- Hire more healthcare practitioners
More practitioners are needed right now to handle the surge in demand for cancer care services. Some jurisdictions are hiring back retired nurses, incentivizing currently employed technicians and practitioners, and bringing more nursing students and international trainees into the system.
Alberta, for instance, hired 648 student nurses to provide care at hospitals and alleviate staff shortages, and Quebec is recruiting 1,000 international nurses.
- Introduce processes to maximize system performance
Within the cancer system, some providers may be significantly backlogged while others have capacity. Centralizing the intake of cancer patients for diagnostic procedures and discrete treatments could relieve specific pressure points and maximize available capacity system-wide.
Another way to address this is to deliver low-risk, frequent activities, such as colonoscopies and imaging, in outpatient settings, and to move less-intensive non-oncology procedures such as cataract and hernia surgeries into ambulatory surgery centres to free up hospital rooms for cancer patients. The Ontario Medical Association, for instance, is looking at creating integrated ambulatory centres that would focus on specific day surgeries which may allow them to deliver care more efficiently than inside a hospital.
- Increase training, activate recruitment and improve retention
The multi-year training requirements for technicians, nurses and physicians limit how quickly the system can bring on new cohorts of healthcare professionals. Raising enrolment limits on Canadian nursing programs would help to address this, as would modifying immigration policies, in an ethical way, to fast-track qualified cancer care workers from other countries. As noted above, this is already starting to happen in parts of Canada.
Another solution is to introduce training that allows health professionals to work at the maximum of their scope of practice. For example, British Columbia has developed a General Practitioner in Oncology program to strengthen the oncology skills of non-specialist physicians so they can deliver chemotherapy in rural and remote communities and relieve the pressure on urban cancer centres and their staff.
Learn more about the importance of keeping a focus on cancer
Burnout and attrition among cancer care providers and other healthcare professionals must be addressed quickly or the already-stretched cancer system will struggle to meet patient needs as the pandemic continues.
Understanding the actions needed and innovations already underway can help ensure health system leaders and partners can move quickly and collaboratively to address these significant challenges – which is critical because, with cancer, time is of the essence.
Find out more in The road to recovery: Cancer in the COVID-19 era, available here: https://www.partnershipagainstcancer.ca/topics/cancer-in-covid-19-era/summary.
Dr. Craig Earle is CEO of the Canadian Partnership Against Cancer




