By Stephanie Lau, Andrew Tu, and Certina Ho
At the senior home this morning, Marie noticed that her hands were shaking more than usual. She just thought her Parkinson’s was getting worse today, but she progressively felt more lightheaded. When the nurses came to assist for her daily walk, they found her collapsed by the foot of her bed. Marie was immediately transferred to the closest hospital and her admitting diagnosis was determined to be hypoglycemia, which was likely caused by the insulin therapy that she used to manage her diabetes.
Hypoglycemia is defined as low blood glucose levels of less than 4 mmol/L for patients with diabetes being treated with either insulin or an insulin secretagogue (i.e. medications that help our body make and release insulin); while normal fasting blood glucose (FBG) levels are within 4-7 mmol/L. Patients can measure their blood glucose levels through with the use of self-monitoring device (e.g. together with the use of blood glucose test strips) that can be purchased from any pharmacy. The effects of hypoglycemia can be severe and potentially fatal if untreated; therefore, timely and quick recognition and management of hypoglycemia are critical to improve patient safety and outcome.
Recognizing hypoglycemia: Signs and symptoms
In the above case scenario, we saw Marie experiencing some signs of hypoglycemia, such as shakiness, lightheadedness, dizziness, and eventual unconsciousness, but other symptoms of hypoglycemia may include hunger, poor concentration, confusion, irritability, sweating, and increased heart rate, as well as more severe effects such as seizures, coma, and death if untreated. Since the effects of hypoglycemia are rapid, it is, therefore, often considered a medical emergency. (For further information regarding signs and symptoms of hypoglycemia, refer to the 2018 Diabetes Canada Clinical Practice Guidelines: Hypoglycemia, available at http://guidelines.diabetes.ca/cpg/chapter14#sec5)
Populations at risk
In addition to the potentially severe consequences of hypoglycemia, the increasing prevalence of populations at risk of diabetes further demonstrate the need for awareness and education on hypoglycemia management. Populations at greatest risk of hypoglycemia include patients with diabetes who use certain types of anti-diabetic medications (such as insulin and sulfonylureas) as well as those who exercise a lot, consume alcohol, undergo fasting, or have renal impairment.
Managing hypoglycemia
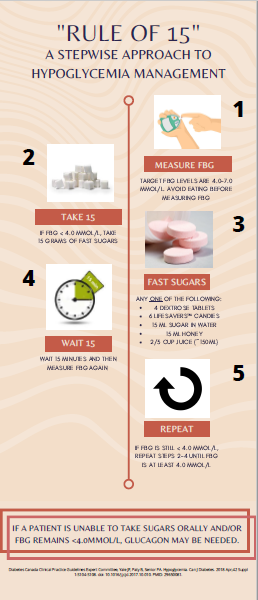
“Rule of 15”
If a patient is experiencing symptoms of hypoglycemia, it is important to measure the blood glucose levels immediately. If the reading is less than 4 mmol/L (and as mentioned above, our target FBG is 4-7 mmol/L), the “Rule of 15” should be employed immediately (Figure 1). If the patient is unconscious and unable to take anything orally (i.e. by mouth), glucagon may be needed. Glucagon is a regulatory hormone that can rapidly increase blood glucose levels in our body. It is available as an subcutaneous, intramuscular, or intravenous injection; and it is also available as an intranasal spray.
“Five to Drive”
Use the “Five to Drive” rule for safe driving: Ensure your FBG is at least 5 mmol/L for at least 40 to 60 minutes prior to driving. If your blood glucose is below 4 mmol/L, apply the “Rule of 15” (Figure 1). If you plan to drive for a long period of time, it is best to take FBG readings every 4 hours to ensure driving is safe and appropriate. Having regular meals, snacks, and taking breaks during a long driving trip may also help. (For further information regarding diabetes and driving, refer to the 2018 Diabetes Canada Clinical Practice Guidelines: Diabetes and Driving, available at http://guidelines.diabetes.ca/cpg/chapter21.)
Other Lifestyle Considerations: Alcohol and Exercise
| Alcohol Consumption | Physical Activity |
| · Alcohol can impair the liver from releasing glucose into the blood, and this effect may last up to 24 hours after alcohol consumption.
· Consuming food or having a meal with alcohol can help prevent hypoglycemia by providing a source of sugar. |
· Exercise consumes glucose and can lower blood glucose levels.
· Avoid exercise immediately after insulin administration. Careful timing of meals and insulin with exercise is necessary to avoid hypoglycemia episodes. · Monitor FBG before and after exercise. For prolonged exercise, it is best to measure FBG during exercise and adjust insulin doses accordingly. Apply the “Rule of 15” (Figure 1) to ensure safe engagement (or re-engagement) in physical activities. |
For further information on diabetes and hypoglycemia management, refer to the full 2018 Diabetes Canada Clinical Practice Guidelines along with the 2020 Updates at http://guidelines.diabetes.ca/cpg.
Stephanie Lau and Andrew Tu are PharmD Students at the Leslie Dan Faculty of Pharmacy, University of Toronto; and Certina Ho is an Assistant Professor at the Department of Psychiatry and Leslie Dan Faculty of Pharmacy, University of Toronto.