Hospital- police partnership supports people experiencing #mental health crises with #mobile crisis intervention teams
“Today, I was dead set on taking my own life and was certain beyond any doubt that anyone could possibly discourage me. I would like to thank the MCIT who managed to get me to take this one step at a time and to give myself credit, and for believing in me. It meant more than words can express. I can tell you without a doubt that having emotional support and protection available is more important than any of the medication being administered to help me emotionally.” MCIT Client
Every year, Toronto Police Service (TPS) receives over 24,700 calls about incidents involving emotionally disturbed people, many who are facing mental health crises. Some incidents result in unnecessary emergency department use, incarceration, injuries or fatalities. One strategy to support such individuals in crisis is mobile crisis intervention teams (MCIT).
The City of Toronto MCIT model partners a mental health nurse with a police officer as a secondary response unit to 911 crisis calls in the community. The teams are available for approximately 10 hours per day, 7 days per week. The team has been found to respond to calls in a respectful and supportive manner. In a 2014 study, the Centre for Research on Inner City Health (CRICH) found that consumers valued the support and positive interactions they had with the teams.
MORE: LET’S RID THE WORLD OF SUICIDE
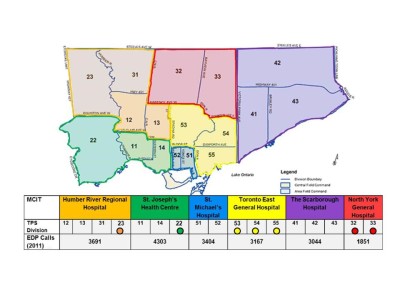
The City of Toronto MCIT program was developed through funding from the Toronto Central LHIN and in partnership with the Toronto Police services and six hospitals. The model was based on recommendations from a cross-sectoral steering committee that proposed the expansion of teams, increased standardization across existing teams and improved data collection for performance monitoring. Today 17 police divisions are covered by 10 MCIT teams, and a program dashboard is used to monitor key indicators.
What are the outcomes of the MCIT model? Four clear benefits to clients and families have been identified.
- Enhanced access to care. The city wide model provides access to an additional 1.3 million Torontonians.
- Decreased stigma through the provision of sensitive care. The respectful and caring approach by the MCIT influences the way clients respond and together the nurse’s compassionate approach coupled with the officer’s firm authority make a difference in safely de-escalating crisis situations.
- Avoidance of tragic outcomes. Timely intervention for clients who are suicidal makes a difference between life and death. Over 27% of the calls in 2014 were associated with suicidality.
- Support and capacity building for families in crisis. Letters from family members and research findings indicate that MCIT have helped them learn how to better manage a mental illness through role modelling, coaching by the nurse and referrals to community resources for ongoing assistance.
MORE: PREVENTING INJECTION DRUG USE
Feedback indicates that the one-on-one care that the nurse is able to provide in a crisis situation to both the individual patient and family members is invaluable in helping them to reshape their lives. The ability to link individuals to local community resources provides timely access to appropriate supports for both current and future crisis situations and in turn avoids unnecessary emergency department visits.
The MCITs are increasingly being recognized for their contribution to the Toronto crisis response system. In May of this year, Sharon Lawlor, MCIT nurse at #Toronto East General Hospital and St. Joseph’s Health Centre was named “Nurse of the Year” in the 2015 Toronto Star Nightingale Awards.
- For more information regarding the City of Toronto MCIT Program, please visit https://www.torontopolice.on.ca/community/mcit.php.


