By Katherine Nazimek
with files from Monica Matys
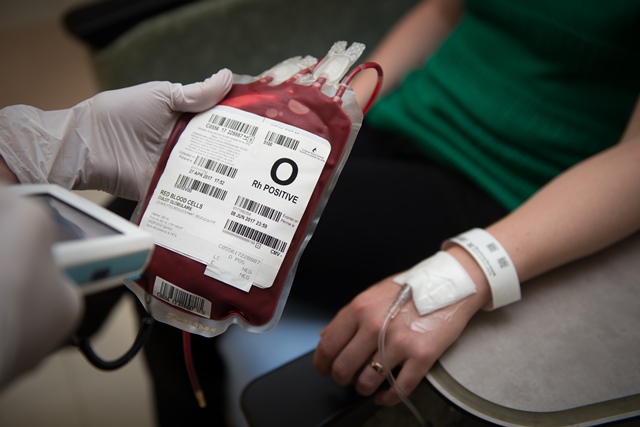
Being admitted to hospital goes hand-in-hand with a lot of testing, from pathology samples to check for cancer, to blood tests and transfusions. A single sample could change someone’s life: proof that they are illness-free, or a diagnosis that triggers the start of treatment. One mislabelled specimen or inaccurate test could have fatal consequences.
Over the past few years, Sunnybrook Health Sciences Centre has expanded its use of innovative technologies to make sure those tests and transfusions are done more accurately, beginning with sample collection.
In the past, patients were given wristbands with stamped patient information or identification. These wristbands were manually checked by hospital staff to make sure the right test or procedure was being done. But there was always room for human error.
“One in 2,000 times they would have either the wrong name or the wrong blood in the tube, and you would have an error,” says Dr. Jeannie Callum, Director of Utilization for the Department of Laboratory Medicine & Molecular Diagnostics at Sunnybrook. “That’s just what the human error rate is for sample collection, and it’s very consistent hospital to hospital.”
Barcoding systems have been increasingly used in hospitals around the world to cut the risk of patient misidentification. And in 2016, Sunnybrook began to roll out a hospital-wide barcoding system, called electronic Positive Patient Identification (ePPID), to help prevent these errors for both lab samples and blood transfusions.
With ePPID, patients are issued a barcoded wristband that, when scanned, provides the patient’s information and a unique patient identifier. This allows staff to confirm the patient’s identity and label samples at the bedside, track collection in real time and, where applicable, ensure that the correct blood product is transfused.
“This approach reduces the risk of patient and specimen misidentification significantly; to one in every 15,000, from one in 2,000,” says Callum.
Next comes blood testing.
After blood samples are collected and barcoded, they are delivered to Sunnybrook’s new Core Laboratory on foot or through the pneumatic tube system – a two-way highway that lives between the walls of Sunnybrook and connects the lab to 25 patient care areas throughout the hospital.

Within the 15,000 square-foot Core Laboratory is Ontario’s first end-to-end automated biochemistry lab, where blood samples can go from receipt to result uninterrupted and without ever being touched by an operator.
“Previously, laboratory staff would need to intervene at each step of the testing process, loading and unloading specimens onto specialized instruments that would prepare samples and conduct testing,” says Lisa Merkley, Director of Laboratory Medicine & Molecular Diagnostics at Sunnybrook.
“Less human intervention means less opportunities for error,” adds Dr. David Hwang, Chief, Laboratory Medicine & Molecular Diagnostics. “It means increased efficiency, faster turnaround times, and the ability to reallocate resources to provide better quality of care.”
In the new lab, a highly specialized team of technologists, technicians and biochemists work around the clock, utilizing the Roche state-of-the-art laboratory automation system for both testing and specimen archiving. Together, the experts and the machine process approximately 4.5 million tests per year for Sunnybrook patients, community hospitals, government and research agencies, and private laboratories throughout central Ontario.
Take a look behind the scenes of the automated biochemistry lab at Sunnybrook.ca/mag.
Katherine Nazimek is a Communications Advisor at Sunnybrook Health Sciences Centre.

