
By David Musyj
I was looking back at my first memo to our team at Windsor Regional Hospital, dated January 22, 2020.
It states, “Recently there has been a Novel (new) Coronavirus first identified in Wuhan, Hubei Province, China. There are estimates of over 400 people infected worldwide and nine reported deaths. The first case was confirmed in the United States yesterday.” It goes on to provide clinical details known at the time and ends with, “Our pandemic response team will be meeting regularly as the situation evolves to ensure we are ready and provide updates on a regular basis.”
Closing in on three months later, it feels like a decade has passed.
Since January 22, 2020, through to today, I start off my day by sending a daily update to the team on what is now known as COVID-19 with local updates, international updates and things for the team to remember or get ready for.
Ever since January 22 through to today, our team has responded with flying colours. They have applied their years of experience, education, training, drills and table-tops to be in the best position possible to address what is in front of us and our community, province and nation.
Our motto from the start has been from the words of Maya Angelou: “hoping for the best, prepared for the worst, and unsurprised by anything in between.” We have not only been preparing for the possible surge of local patients in the various models and projections, but also preparing to help support the rest of the province if there is a “hot spot” elsewhere in the province that needs our support. By the time this article is printed, we should have a better sense of whether we have been able to individually and collectively #flattenthecurve.

For our region, the impact of not flattening the curve would be dramatic. With a population in Windsor and surrounding Essex County of approximately 400,000, having 50 per cent of the population infected with COVID-19 and even the five per cent of that number being hospitalized into critical care is staggering.
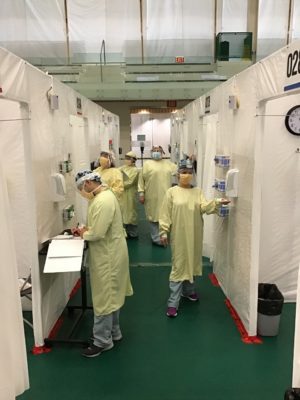
As one of our team members stated, “We are not preparing for a battle. We are preparing for a war.” On an infrastructure side, from massive internal changes in order to maximize capacity, pausing scheduled surgeries, to creating tarpaulin tented isolation rooms and converting them into negative pressure rooms, to creating a COVID-19 assessment centre in a weekend, to creating screening stations for all staff and visitors/patients when they enter, to creating a field hospital at a local community college, to addressing possible limited morgue capacity, the war preparations were well under way. On a staffing side, to educate all of our staff on the pandemic plan, hiring recently retired staff, cross-training staff into medicine/critical care areas, hiring current nursing students to help support the team, and completion of mask fit testing for some 5000 staff members, the war preparations were under way.
At the same time all this was happening, Ontario health care was undergoing a dramatic change in operational structure moving towards an Ontario Health model, with the province divided up into five regions. One would think this would be like changing a tire on Highway 401 going 100 km/hour. However, this transition to Ontario Health could not have come at a better time. Ontario created a provincial command table made up of two representatives from each of the five new Ontario Health regions. The West region, which our hospital is now a member of, is one of the largest geographical regions in the province reaching from Windsor to Mississauga and through the Bruce/Grey peninsula. Under the expert stewardship of West region CEO, Bruce Lauckner and Dr. Thomas Stewart, St Joseph Health System and Niagara CEO, who sit on the provincial command table, a group of three other hospital CEOs, including myself, non-hospital sector leaders and public health meet daily and share issues back with their sub-regions and vice versa. Within the former Erie St Clair LHIN sub-region, all hospitals and non-hospitals have various “tables” that meet multiple times a week to share information and consistency in the sub-regions, across the greater West region and then across the whole Province. These “tables” ensure voices on topics like operations, critical care, ER, communication, human resources, bio-ethics, infection control, supplies and lab are sharing information, are heard and are consistent. At the same time, on the non-hospital primary care, long term care/retirement homes, EMS, home care/community care, digital and mental health and addiction are in lock step. This is replicated in all five regions. The future for Ontario Health looks bright.
 Even though it looks like we have collectively done well to stem the tide of the war on the front lines by stabilizing acute care admissions and critical care admissions, we are being hit with a flank maneuver trying to attack our most vulnerable populations in long term care, retirement homes, homeless populations, migrant workers and other congregate settings. We have to take this issue head on. We cannot afford to sit back and have our most vulnerable become, as Governor Cuomo has stated, a “feeding frenzy” for COVID-19. Action needs to be taken.
Even though it looks like we have collectively done well to stem the tide of the war on the front lines by stabilizing acute care admissions and critical care admissions, we are being hit with a flank maneuver trying to attack our most vulnerable populations in long term care, retirement homes, homeless populations, migrant workers and other congregate settings. We have to take this issue head on. We cannot afford to sit back and have our most vulnerable become, as Governor Cuomo has stated, a “feeding frenzy” for COVID-19. Action needs to be taken.
The community support for health care workers has been breathtaking and will not be forgotten. They have rallied around a team who are “people too” and have the same anxieties and concerns of the general public. However, our health care team knows this is the time for them to stand strong for our community and lead them through this pandemic. We have cried together, laughed together, but kept our social distancing in doing so.
Having been around for SARS, the difference from that era to COVID-19 in information sharing, communication, teamwork and speed of making changes is staggering.
I read a funny yet truthful tweet the other day: 2020 is a unique leap year. It has 29 days in February, 300 days in March and five years in April.
Let’s hope the months feel shorter as the days get longer this summer.
David Musyj is President and CEO of Windsor Regional Hospital.

