By Elise Copps
35-year-old woman, unrestrained driver of an all-terrain vehicle. Rolled multiple times into the ravine, approximately eight feet down an embankment. Blood pressure is 90/60, pulse 110, respiratory rate 40. She has decreased breath sounds on the left side and an unstable pelvis. ETA is 9 minutes.
You receive this briefing from paramedics about a patient who’s en route to your hospital. What do you do?
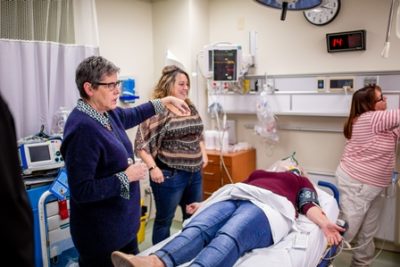
This high-stakes situation was played out at a recent simulation training event at a community hospital in our region. A trauma scenario like this one is stressful for everyone. It can be particularly tough for smaller hospitals. They don’t see trauma cases as often as the lead trauma hospital, which makes it difficult to practice the rhythm of these critical events.
 That’s where realistic simulation training comes in. Last year, Dr. Paul Engels, a trauma team lead with Hamilton Health Sciences’ Hamilton General Hospital (HGH), launched the Rural Trauma Team Development Course (RTTDC) in our region. The course was developed by the American College of Surgeons Committee on Trauma as a way to educate trauma care providers in smaller hospitals, so these providers can learn a standardized approach.
That’s where realistic simulation training comes in. Last year, Dr. Paul Engels, a trauma team lead with Hamilton Health Sciences’ Hamilton General Hospital (HGH), launched the Rural Trauma Team Development Course (RTTDC) in our region. The course was developed by the American College of Surgeons Committee on Trauma as a way to educate trauma care providers in smaller hospitals, so these providers can learn a standardized approach.
“Eventually, everyone in the region will be working from the same “song book” so to speak,” says Dr. Engels. “By providing the RTTDC, we have a certified and standardized approach to teaching within the Central South region.”
Hamilton General Hospital (HGH) is the lead trauma hospital for Central South Ontario. The hospital has a robust trauma program, and the majority of trauma patients in the region are sent directly to HGH for care. As the lead trauma hospital, HGH is responsible for providing education within the region, and working with regional partners to improve the trauma system. This training is part of that work.
So far, the team has hosted four training sessions at community hospitals across our region. During training, the course attendees learn the components of trauma care and what to do under different circumstances. Each session typically includes a simulation of a pediatric, adult, and geriatric trauma case.
The patient arrives in the emergency department. Blood pressure is 88/64, pulse 120, respiratory rate 40 and shallow. Cervical collar and long backboard have been applied. A single attempt at IV access was made and this was unsuccessful. Oxygen has been applied via nonrebreather mask. No medications been given. The patient complains of severe pain in her jaw and in her left chest, abdomen/pelvis and flank.
Now the team has to assess and act. What are the patient’s exact injuries? What equipment is available, and where is it located? A scenario like this one prompts the providers to think about the resources they can make use of in dire circumstances.

“The goal is to get them thinking about how they work together,” says Dr. Engels. “What works well? What are their challenges and why? The focus is on them as a community hospital providing trauma care.”
Because the training takes place in the community hospital, the team gets authentic experience. They’re working with the space and tools they’ll have when a real trauma case comes through their doors. It allows them to test their action plan under the watch of seasoned trauma experts. Research shows this standardized trauma training speeds transfer time from a community hospital to a trauma centre.
“Effective treatment and speedy transfer to a regional trauma centre improves survival rates and recovery,” says Barb Klassen, Trauma Program Coordinator at HGH. “This program emphasizes early communication with the regional trauma team at HGH. That ensures patients get the best possible care at their community hospital, and can be transferred quickly to our hospital for specialized trauma care.”
The team leader calls the regional trauma hospital. A list of all currently recognized injuries is given. The trauma team lead advises on the best approach to stabilizing the patient for transfer. Within an hour, she is loaded into an air ambulance for transfer to Hamilton General Hospital.
So far, the training sessions have been very well received by participants. They get a chance to provide feedback to the trauma team about what works and doesn’t work with current processes. They are not only learning, but also improving the system as a whole. Early data suggests the program is also moving the needle on patient transfer times. The trauma team plans to continue offering three to four sessions each year to community hospitals in our region.
Elise Copps is the Public Relations Specialist at Hamilton Health Sciences.

