The goal here is to be better 10 minutes from now than we were 10 minutes ago,” said Dr. Glenn Posner, director of The Ottawa Hospital’s (TOH) Simulation Patient Safety Program. “If this same scenario happens in the next bed 10 minutes from now, we are going to be a well-oiled machine.”
Since 2014, TOH has been improving safety, fostering education, and sharing knowledge through their Simulation Patient Safety Program (SPSP). To learn what sets it apart, we spoke to the program’s director, Dr. Posner; lead medical facilitator, Dr. Doran Drew; and simulation educator and nursing lead instructor, Jennifer Dale-Tam.
The SPSP focuses on simulation training that takes place in the hospital or other clinical setting. It’s a part of the organization’s Corporate Strategy, which is one of the elements that make TOH’s program so unique.
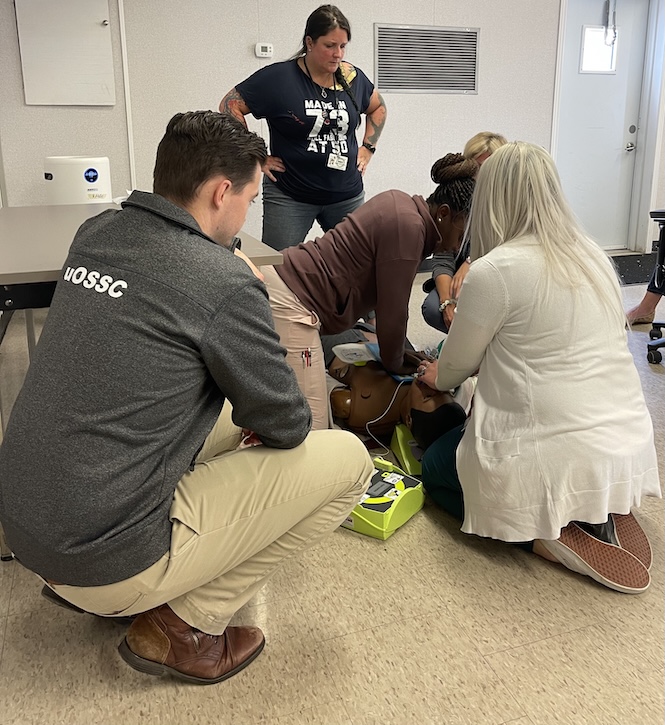
Promoting interprofessional collaboration, the training resembles real-life crisis scenarios by involving real teams responding to simulated patients, while fulfilling requirements from Accreditation Canada. Simulation training also reinforces the importance of practicing and highlights what can be optimized in the healthcare system.
Dale-Tam emphasized the importance of simulation training: “It is the pinnacle of the application of knowledge and skills previously learned by the health professions.” It is a space to learn and take risks without any harm to real patients and prepares health professionals by practicing, communicating and working together as a team ensuring safe, quality patient care.

Promote Interprofessional Collaboration
At HIROC, having the opportunity to hear voices from across the healthcare system is at the cornerstone of our commitment to share valuable knowledge, all with the goal of scaling lessons learned. This is why we want to highlight interprofessional collaboration, which is key to simulation training and clinical practice, and the role of nurses, who are crucial to the healthcare system and driving safety.
“Historically, much of our training is done in silos and research is showing this does not provide the best outcomes for the patient. All health professions have a unique body of knowledge, and many a particular philosophy when it comes to patient care, but we need to understand each other and how to collaborate to achieve optimal patient outcomes,” Dale-Tam said.
Address Latent Safety Threats
The SPSP also enables the discovery of latent safety threats (LST) that could impact quality patient care. LSTs that may not have been found otherwise can then be fixed proactively. For example, in TOH’s first simulation training session in 2014 of a cardiac arrest, they discovered the crash cart defibrillator had the incorrect pads on which would have delayed patient care in a real situation.
Similarly, simulation training offers a way to test protocols and procedures before implementing them clinically to ensure safety, and it supports TOH’s goal of creating a patient safety culture.
“One of the things we’ve been seeing when we’ve been doing our in-situ simulations is the feedback is resoundingly positive,” said Drew. “The spirit of this is actual teams practicing together just to see what things work and what things don’t, identify system issues that are going to be barriers to patient care, and provide our teams with education while they’re at work.”
Debriefing Matters
Another key aspect of the program is debriefing. In real situations, there is little time to stop and reflect between patients, so debriefing in training offers a safer, low-stakes environment where participants feel comfortable talking about the case. Debriefing is also a main component of coaching in various high-performance fields, such as athletics and aviation – it’s all about improving learning. Medical education literature shows high-performance healthcare teams can benefit from it too.
“It’s so important to reflect on what you did well and what could’ve gone better, and we don’t do it enough in real cases because the hospital is a runaway train. You jump on for your shift and jump off at the end of your shift, but it’s always going. When you finish a case, there’s another case waiting,” Posner said.
Stay Curious and Seek Training
“My advice to someone who is building up a program at a different hospital would be encouraging them to stay curious and explore the things they’re seeing because often it’s going to relate back to their underlying mission,” Drew said. “One of the nice things about the in-situ programs is you’re on the ground level working with people who are directly providing care, so you often are in a nice situation where you can do some root cause analysis.”
Dale-Tam recommended formal or informal training programs for simulation-based education. “There are many in Canada from organizations like Simulation Canada, the Royal College of Physicians and Surgeons of Canada, or the Canadian Association of Schools of Nursing. Looking for a mentor in the area helps too.”
She also highlighted how developing your simulation facilitation skills is critical for simulation education. “There is research coming out that learners who have participated in simulation scenarios that are facilitated by untrained faculty may develop PTSD-like symptoms even though that is not the intent of the facilitator. Participating in simulation can be scary; some may see it as a test or threat to their professional identity. A trained facilitator will put strategies in place to create that safe space for learners to take risks and see the associated outcomes before taking it into clinical practice.”
Learn more about TOH’s Simulation Program at uossc.ca.
Gillian Brandon-Hart is a Communications & Marketing Specialist at HIROC.