Many cancer patients are living longer, thanks to new and better treatments and cures made possible through research.
But what about life after cancer treatment? There’s an emerging area of research aimed at helping cancer survivors enjoy the very best quality of life in the months and years after completing treatments like chemotherapy, radiation therapy and surgery.
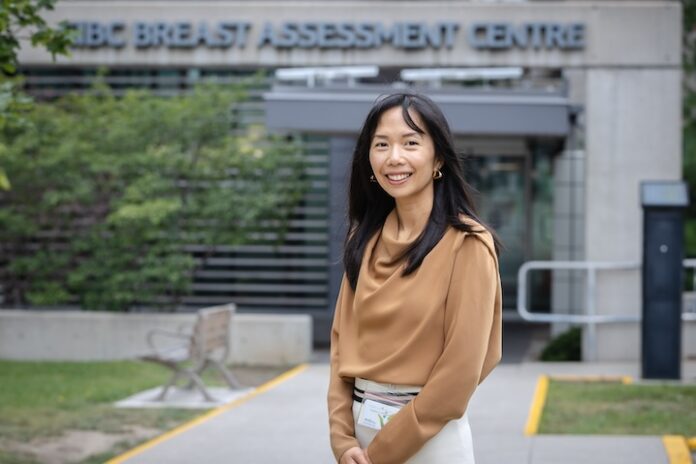
Researchers leading these quality-of-life studies include Hamilton Health Sciences (HHS) psychologist Dr. Karen Zhang, who cares for cancer patients at HHS Juravinski Hospital and Cancer Centre (JHCC). Zhang is also a researcher with the Escarpment Cancer Research Institute, a joint institute of HHS and McMaster University. As a psychologist, Zhang is especially interested in research that understands and addresses the psychosocial aspects of cancer care.
“I see a lot of room for research and innovation that explores how to help people live better with cancer, as well as after cancer treatments have ended,” says Zhang. “I’m especially passionate about studies aimed at developing programs to help people manage better.”
Life after breast cancer
Projects that Zhang is currently working on include the breast cancer research study, I-CAN Manage Cancer Pain. Zhang is the co-principal investigator along with Dr. Greg Tippin, a psychologist with the HHS Michael G. DeGroote Pain Clinic, the largest academic university-affiliated pain clinic in Canada.
This pilot feasibility study brings together HHS health-care professionals from the JHCC and the pain clinic to explore pain management for breast cancer survivors in the months and years after finishing treatment. Health-care professionals involved in the study include psychologists, oncologists, a pain specialist, nurse, physiotherapist and occupational therapist.
“We want to help people better manage their pain, so they can live their best lives,” says Zhang.
Chronic pain
The study, which has the potential to be expanded in the future, focuses on patients diagnosed with Stage 1 to 3 breast cancer who continue to experience pain in the months and years after treatment.
Common reasons for chronic pain include neuropathy – a side effect from chemotherapy that causes tingling or numbness in the feet or hands and can spread to legs and arms. In severe cases, it can affect people’s ability to do everyday activities including returning to work, says Zhang.
People can also experience prolonged post-surgical pain from their mastectomy or incisions. And some medications can also cause pain symptoms.
Vital support
An HHS Foundation grant of just over $48,000 made it possible to hire a research coordinator to help organize the study and recruit participants.
“The importance of supporting research cannot be understated,” says Anissa Hiborn, the HHS Foundation’s CEO.
“Health journeys don’t end once a person leaves a hospital or treatment plan, and Dr. Zhang’s research work in pain management can help so many women in their quality of life after breast cancer. Donor dollars are making a tangible difference in improving our region’s health care and I’m proud of the community’s generosity.”
Virtual sessions
The research team will recruit approximately 30 study participants through the JHCC, Wellwood support centre and the BRIGHT Run fundraiser for breast cancer research.
These study volunteers are divided into three cohorts, each taking part in six-week virtual interprofessional pain management program developed by the study team and modeled a validated chronic pain intervention. The goal of the program is to help survivors better manage their pain symptoms so that they can cope better with the aftermath of their cancer journey.
“Rather than reinventing the wheel, we were able to adapt an already validated intervention program for our study participants,” says Zhang.
Sessions are led by HHS psychologists, nurses, occupational therapists and physiotherapists, and offer strategies for self-managing pain that included exercise, breathing techniques, and relaxation and mindfulness exercises.
“Some strategies are more psychological in nature, while others focus on exercise or information,” says Zhang. “Our study really concentrates on leveraging our expertise to help people cope through self-management.”
Positive feedback
The program hasn’t been fully evaluated yet, as the study is still in the process of data collection. However, verbal feedback from participants has been positive so far. “We’re currently running focus groups with participants to get their feedback,” says Zhang, adding that she appreciates opportunities to collaborate with so many experts at HHS, including her pain clinic colleagues.
Next steps could include a randomized control trial to help determine the effectiveness as standard program for breast cancer survivors.
“There’s a lot we don’t know yet about supporting patients during and after cancer treatment,” says Zhang.
“With my research, I’m trying to identify gaps where our standard clinical services may not be meeting psychosocial needs of patients. That’s where I see a lot of room for research and innovation to help people live better with cancer, and after cancer.”

