St. Michael’s Hospital researcher is launching a first-of-its-kind global trial to test the impact of MDMA, commonly known as ecstasy, on chronic nerve pain compared with a placebo.
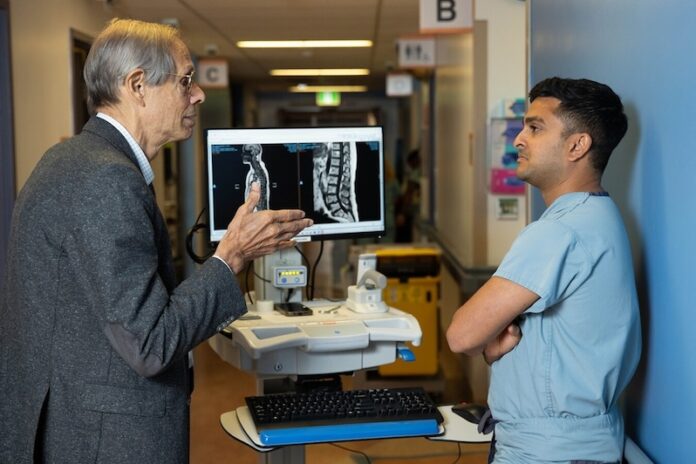
Pending regulatory approval, the St. Michael’s MDMA clinical trial will recruit 30 patients with chronic nerve pain from across Canada. These patients will be randomly assigned to receive either MDMA and psychotherapy or the active placebo methylphenidate, commonly known as Ritalin, and psychotherapy. The trial team, led by Anesthesiologist Dr. Akash Goel, is aiming to start recruitment in January 2025 and completion is scheduled for June 2026. It is the first active-placebo controlled trial of its kind, and Goel recently won $150,000 from the St. Michael’s Hospital Foundation Research Innovation Council to help launch the study.
“Currently, around one in five Canadians suffer from neuropathic pain, and many have no recourse for improvement,” said Goel, noting that common causes of neuropathic pain include diabetes, cancer, surgery and Multiple Sclerosis. “Of these patients, one in five rate their pain as worse than death, so there’s clearly an important need for innovation in this space.”
MDMA, which is short for methylenedioxymethamphetamine, is a synthetic psychoactive drug that works by affecting chemicals in the brain that play key roles in regulating mood, energy and social behavior. MDMA is known for altering mood and perception, and can cause increased feelings of happiness, empathy, energy and can heighten the user’s senses.
First created by Merck in the early 1900s, MDMA was used experimentally to enhance psychotherapy in the 1970s. In the 1990s it became associated with the underground rave scene and is now considered illegal in many jurisdictions, including Canada. Despite its illegal classification, Health Canada allowed limited distribution of MDMA for medical and research purposes in 2022.
In recent years, there’s been renewed interest in studying MDMA as a treatment for pain and mental health disorders, said Goel. The results from a 2023 clinical trial found that MDMA significantly improved symptoms of post-traumatic stress disorder (PTSD) in patients compared to placebo and psychotherapy. The trial also found that MDMA significantly improved pain-related disability for a sub-group of participants with chronic pain. However, the FDA raised concerns with the trial design, in particular, the lack of an appropriate active-placebo, as 90 per cent of patients correctly guessed if they had received MDMA or the placebo.
The St. Michael’s MDMA trial is the most recent study from the Pinnacle Research Group to investigate the effects of psychedelic drugs on chronic neuropathic pain. The Pinnacle Group is conducting similar trials testing the impact of ketamine and psilocybin.
A potential game changer?
Research suggests that MDMA creates feelings of empathy and openness, so that patients with trauma – and living with chronic nerve pain is trauma – can face it more openly, Goel said.
“This is called fear extinction. They’re able to revisit and explore that trauma in a way that helps them understand their experiences,” he said. “This can help them adapt principles of psychotherapy into their daily lives in a more meaningful way and could leave a lasting positive impact on their life.”
There’s also mounting debate over whether MDMA improves neuroplasticity, which is the ability of neural networks in the brain to change through growth or reorganization, Goel adds. MDMA may create an opportunity for someone with chronic pain and unhealthy brain connections to lay down new, healthier neural frameworks, he said.
“I compare it to our aging highway system in Toronto. The highways were built decades ago, and they’re not really set up for the 2020s. What you need to do is lay down a completely new map.
“These are some of the reasons we believe MDMA could be a potential game changer in the area of pain medicine, as well as other mental health disorders.”
MDMA has side effects, including rapid heartbeat, dehydration, blurred vision, fatigue, depression and anxiety. As such, all participants will be doing psychotherapy while in the trial to ensure that they have stable and constant access to mental health supports, said Goel. The trial team will also touch base with participants regularly to see if they are experiencing prohibitive side effects. Patients who show active suicidality or have a history of psychosis will be excluded from the study to prevent serious adverse events, he said.
“Our research group has a solid infrastructure here at St. Michael’s to ensure that we have the right protocols in place, the right drug manufacturer and we develop our network to ensure that this clinical trial can be executed in a safe manner,” Goel said.
An everyday battle
The St. Michael’s pain trials could bring relief to patients like Gabe Ramsay, who’s been suffering from debilitating chronic nerve pain after having elective laser eye surgery in 2018. Following his surgery, Ramsay developed dry eyes and inflammation of his corneas, which eventually developed into corneal neuropathic pain.
“I had a terrible time recovering from the surgery. I’ve had a constant, burning and stabbing pain in my eyes, that’s spread to parts of my face as well,” Ramsay said, noting that his pain drove him to leave work for a few months and even prompted him to decline entering a university Master’s program.
“It’s totally changed my life and everything I do. I’ve been battling it for six years.”
Ramsay had tried different treatments and procedures and even arranged to see a specialist in Boston. Because most of the treatments were not covered by OHIP, he paid for most of them out of pocket.
While he’s made some progress and has returned to work, Ramsay’s still dependent on a number of treatments, including eye drops and medications, which he says make him groggy and affect his short-term memory. He’s still looking for a more effective
treatment.
“There’s a psychological aspect of chronic nerve pain, especially when there are no good treatment options,” he said. “The future is just so uncertain, and the pain can get worse. It can spread. This makes it hard psychologically to prepare for the future or think ahead.”
Goel says Ramsay’s experience is one he commonly sees in patients. “It’s not just the pain, it’s how the pain impacts relationships, careers, families,” he said. “It’s an experience.”