HN Summary
• World-First Remote Robotic Neurovascular Procedure
St. Michael’s Hospital performed the first-ever robotic-assisted neurovascular diagnostic procedure remotely, with the patient at St. Michael’s and Dr. Vitor Pereira operating from St. Joseph’s Health Centre, six kilometres away. This groundbreaking procedure demonstrates the feasibility of performing minimally invasive, endovascular interventions across a network connection.
• Cutting-Edge Technology & Safety Measures
The procedure used a next-generation surgical robotic system from Remedy Robotics, allowing precise catheter navigation while a specialized bedside clinical team supported the patient. Extensive testing and a secure layer-2 fibre optic network ensured patient safety, marking the first human use of this remote-capable system.
• Future of Remote Specialized Care
The initiative, called Cut the Cord, aims to expand remote interventions for life-saving treatments, such as aneurysm repairs and stroke clot removal, bringing specialized care to rural and smaller hospitals. The project reflects a paradigm shift in neurovascular care, where expertise can travel to the patient rather than requiring the patient to travel.
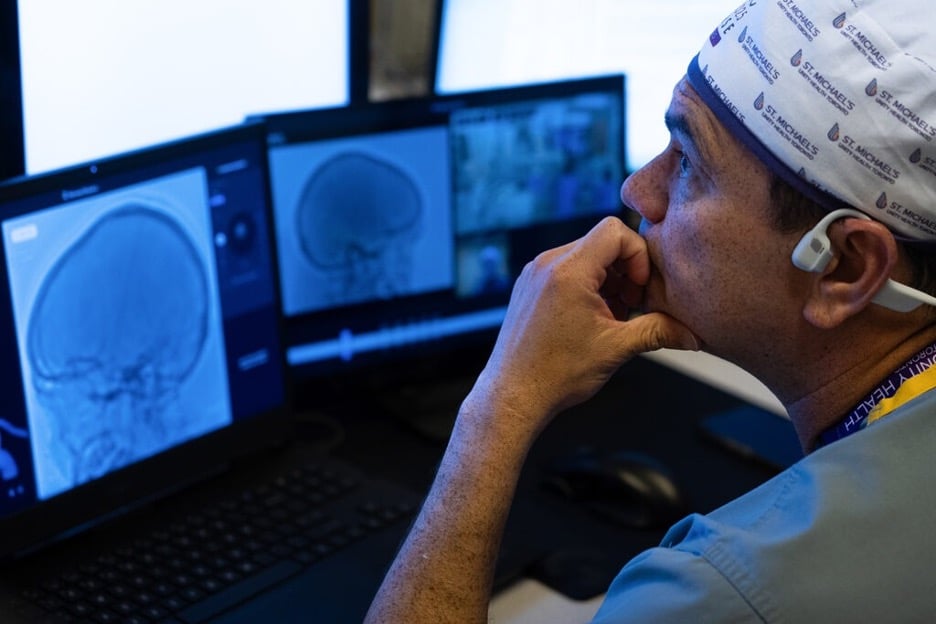
In a world-first, a surgical team at St. Michael’s Hospital in Toronto has performed a robotic-assisted neurovascular diagnostic procedure remotely over a network connection—with the patient at St. Michael’s in the downtown core and the surgeon located at St. Joseph’s Health Centre, a community hospital six kilometres away.
Dr. Vitor Mendes Pereira, a neurosurgeon who specializes in neurosurgical minimally invasive procedures, performed a diagnostic angiogram in two patients located at St. Michael’s while he remained at St. Joseph’s. Both hospitals are part of the Unity Health Toronto hospital network.
Diagnostic angiograms are an important first step in evaluating the blood vessels in the brain for neurovascular diseases, such as stroke, brain malformation and aneurysms. Strokes are a medical condition where the quicker a patient receives treatment, the better chance they have at recovery.


‘We can conquer time’
This act of “cutting the cord” between the robot and the controllers marks a new frontier in neurovascular and stroke care, where life-saving interventions such as the removal of a blood clot from the brain or securing a ruptured brain aneurysm, will be able to be performed remotely.
“Cut the Cord is addressing two main problems: access to medical expertise and time,” said Pereira, the Walter and Maria Schroeder Chair for Neurovascular Interventions. “Our next goal will be to expand remote specialized care and treatments such as brain aneurysm repairs and mechanical thrombectomy—the removal of a blood clot from the brain—to communities that do not have a neurosurgeon or neuro-interventionalist. We can save patients hours of transport time before they receive treatment. With Cut the Cord, we can conquer time.”
This remote procedure was enabled by a new generation of surgical robotic systems developed by Remedy Robotics, which allows minimally invasive endovascular procedures—performed inside blood vessels—to be conducted robotically by a remotely located surgeon with a specialized bedside team. These procedures mark the first-in-human use of this next-generation system.
For the past year, Unity Health and Remedy Robotics teams have been conducting extensive testing and simulations on the network and with the robot to ensure the highest level of patient safety and security.
The ultimate aim, said Pereira, is for surgeons in acute care hospitals and regional stroke centres, such as St. Michael’s, to be able to operate remotely over a high-speed network on patients in rural communities and smaller health centres. These patients would otherwise have to travel hours for time-sensitive specialized care, he said.

Global first cases
In these global first cases, performed in late August, Pereira was stationed at St. Joseph’s and controlled the robot to navigate a catheter through the patient’s blood vessels to perform angiographic imaging to assess where there might be any narrowing or blockages.
Although these initial procedures were diagnostic in nature—meaning the catheters did not enter the brain’s blood vessels—the next step is to use the next iteration of the robotic system to perform remote treatments, which will involve navigating catheters and devices directly into the brain.
At St. Michael’s, the patient was with the robot and supported by a specialized bedside clinical team, including Nicole Cancelliere, RADIS Lab co-lead and Research Program Manager, who played a key role as the bedside robotic medical radiation technologist, ensuring the safe operation and integration of the robotic system. The procedures were conducted over the layer-2 fibre optic internet connection that binds all Unity Health Toronto hospitals.
“Our lab has been advancing local and remote endovascular robotics since 2018. It’s incredibly exciting to see this work realized in remote clinical applications,” said Cancelliere.
“Cut the Cord is a success thanks to the infrastructure and support in place at Unity Health which, together with next generation robotic technology, allowed us to safely complete these cases. We are expanding remote procedures in a stepwise fashion by progressively increasing the distance between the operator and the bedside team, so that we can test each variable independently and ensure maximum safety for our patients.”
“What we’ve achieved here isn’t just a technical milestone – it’s a paradigm shift. The brain and its blood vessels no longer need to wait for geography,” said Dr. Julian Spears, head of neurosurgery and co-principal investigator of a research grant on remote robotics through the St. Michael’s Hospital Foundation’s Angels Den. “With remote robotic intervention, expertise comes to the patient, not the patient to the expert.”
Cut the Cord would not be possible without the support of Unity Health Toronto’s leadership, St. Michael’s Hospital Foundation’s generous community of supporters—including lead donors The Schroeder Foundation, The Rathlyn Foundation and Agnico Eagle Mines Ltd., as well as funding through Angels Den—Remedy Robotics, and the team of pioneering physicians, clinicians, researchers, and technologists, Pereira said.
“For a project of this dimension, you need everybody to be holding hands. We have an incredible amount of support here for innovation, for research, and for transformational technologies,” he said.

