By Dr. Vimal Mishra
The COVID-19 pandemic forced us to reimagine, reorder, and restructure every sector of society. In almost all instances, technology has been at the heart of our adaptations. Nowhere has this transformation been more pronounced than in the practice of medicine.
As practitioners responded to the pandemic, telehealth and virtual care adoption accelerated dramatically around the globe — to keep patients and healthcare providers safe and to increase access to care.
It was an acceleration that, while challenging at the time, has largely delivered positive results. Many patients have shown their enthusiasm for virtual care, appreciating its flexibility. And as physicians, being able to offer this kind of flexibility is not only a point of pride, but a change that often allows us to practice better medicine. Managing virtual care addresses the universal challenge of a future enabling five key “rights:” the right care, at the right time, in the right setting, by the right physician or clinician, using the right modality (such as phone appointments or video calls).
Many of us are seeing the value of virtual care firsthand. A study from the Canadian Medical Association reinforces what I’ve heard from colleagues who practice in Canada and the U.S. In it, 94 per cent of physicians polled said they currently provide virtual care (including by telephone, video conferencing, email, and other modalities). More importantly, 70 per cent said they believe virtual care improves patient access and enables quality, efficient care.[1]
A framework to measure the value of virtual care
In response to some of these positive results, we’re seeing more appetite to invest in virtual care, including in Canada. Each of the provinces and territories have action plans to expand virtual care offerings in their jurisdictions.
These investments in virtual care will play an important role in reducing backlogs for routine procedures and check-up appointments. Streamlining the more routine concerns helps clinicians prioritize the patients with urgent matters.
However, as the medical community and policymakers decide what the future of virtual care should look like, it raises questions around evidence (namely around value, equity, and access). These are not impossible hurdles – and they’re ones worth conquering.
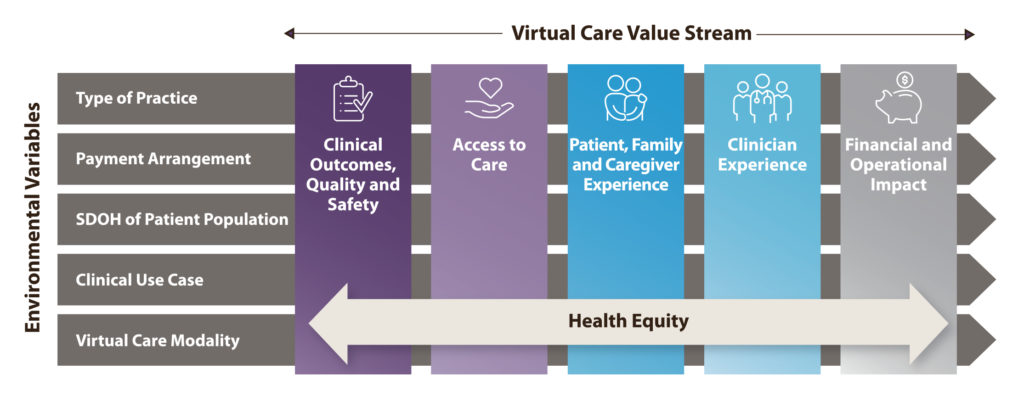
To support clinicians and policymakers alike, the American Medical Association created a framework for measuring the value of virtual care. It considers how virtual care programs may generate benefits for patients, clinicians, and society – all in the context of the post-pandemic “return on health.” Care providers looking to develop and assess new remote care models can use this framework to guide their decision-making on how they use virtual care. Policymakers can do the same, using it to inform coverage and payment decisions, and support the establishment of regulations that work.
The framework includes six value streams, which it then uses to consider the different factors that may influence those value streams, including the type of practice and modality of virtual care (see below).
Measurement across these value streams allows for a better picture of the true value of digitally enabled care. Some health systems are already using it with success. VCU Health in Virginia, for example, used this framework to evaluate the impact of its virtual care model on psychiatry care access. VCU Health Psychiatry practice saw 120% more patients using telehealth (compared to pre-pandemic in-person model), while retaining equitable access. The no-show rate among psychiatry visits declined from 11% pre-pandemic to 6% post- pandemic as virtual visits went from <1% to more than 80% of total visits. Patients were less likely to miss their telepsychiatry appointment because of the improved convenience of conducting a virtual visit.
In using the framework, VCU found ways to reduce wasted time slots. It also gained better insights into health equity questions. Including virtual solutions was found to provide equal levels of care among age groups, despite concerns about older, less tech-savvy patients potentially experiencing more barriers.
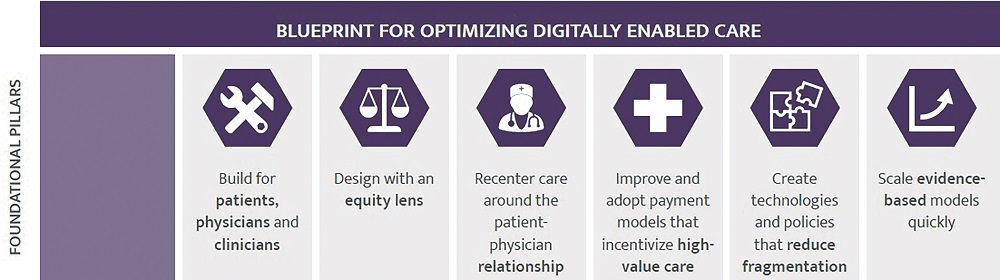
Any conversation around virtual healthcare needs to consider how we measure its value in building stronger, integrated and digitally enabled health systems that empower the right care. Effective decisions about the future of virtual care cannot happen in the context of outdated systems or limited measures of success. A part of this investment often overlooked is the standardization of medical coding which enables the interoperability of treatment regardless of care setting. This coding foundation can not only capture all care, but it can use data sets to help to optimize the efficiency of the system itself.
Many measures of virtual care have been short-term or focused on dollars and cents, rather than its potential to be truly transformative for patient and clinician experience. Realizing the full potential of digitally enabled care will require fundamentally rethinking how care models are designed, implemented, and scaled – and how we measure their impact.
Medicine is changing. The future of care delivery must change, too.
[1] Virtual care in Canada: Progress and potential (report of the Virtual Care Task Force). Canadian Medical Association. https://www.cma.ca/virtual-care-canada-progress-and-potential-report-virtual-care-task-force. Published February 2022. Accessed December 2022.