By Carol Nguyen and Certina Ho
Medication errors can occur at transitions of care, such as hospital discharge, following-up with a specialist or family doctor, and updating medication regimens at the pharmacy. Incidents often occur when there are medication changes that are not properly communicated among healthcare providers within the circle of care of the patient.
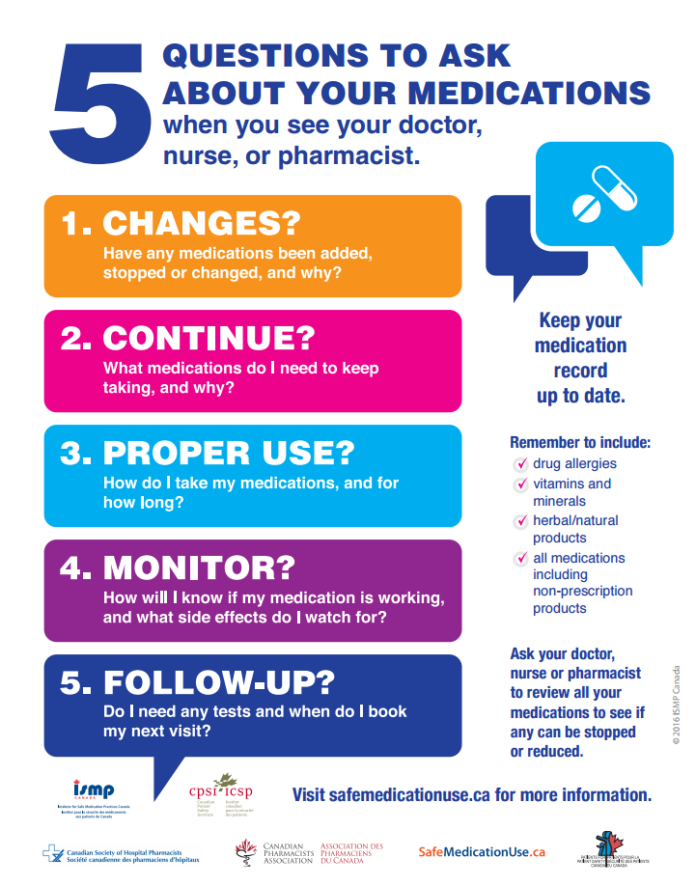
The “5 Questions to Ask About your Medications” is a tool designed for patients and healthcare providers to use as a guide when discussing changes in medications. These questions will help both patients and caregivers start a conversation about their medications and become knowledgeable about their medication therapy management.
Below is a patient case scenario that is used as an example to illustrate the application of this tool.
“A patient admitted with uncontrolled hypertension had been discharged from hospital with changes to her blood pressure medications. She was sent home with a new script for Tiazac®XC 120 mg once a day and advised to stop her metoprolol which she had been taking before admission. She filled the prescription and started the new medication. One week later, she had a follow-up visit with the family doctor, who was unaware of the recent changes in hospital and increased the dose of metoprolol, which had previously been stopped. The metoprolol prescription was filled. The patient was re-admitted to the hospital a few days later due to a low heart rate and it was discovered that she was taking both Tiazac®XC and metoprolol. Her metoprolol was discontinued; she was stabilized and discharged home on Tiazac®XC.”
The opportunities for the patient and healthcare providers to use the tool in this case could have been at the moment of discharge from the hospital, at the family doctor’s office, and at the community pharmacy. For the purposes of this demonstration, the questions will be applied to the patient when she was discharged from the hospital the first time.
- CHANGES?
- Have any medications been added, stopped or changed, and why?
- “ Your metoprolol has been stopped and we are starting a new medication called Tiazac®XC. Your blood pressure was not well controlled on the dose of metoprolol you were on. Therefore, we have switched you to a different agent that will hopefully work better for you.”
- Have any medications been added, stopped or changed, and why?
- CONTINUE?
- Which medications do I need to keep taking, and why?
- This would be the opportunity to ensure that you (as the healthcare provider) and your patient are on the same page about which medications they need to keep taking.
- Assess the appropriateness of the patient’s other medication(s) and explain which ones can be continued safely with the new medication, Tiazac®
- Which medications do I need to keep taking, and why?
- PROPER — USE?
- How do I take my medications, and for how long?
- “Let’s review the new medication – Tiazac®XC– it is to be taken once daily at bedtime and it will be continued long-term, as long as it is well-controlling your blood pressure and you are tolerating it well.”
- How do I take my medications, and for how long?
- MONITOR?
- How will I know if my medication is working, and what side effects do I watch for?
- “You want to meet your blood pressure target of less than 140/90 mm Hg and to avoid the medication’s side effects. Side effects of Tiazac®XC include, for example, dizziness, lightheadedness, and edema.”
- How will I know if my medication is working, and what side effects do I watch for?
- FOLLOW-UP?
- Do I need any tests and when do I book my next visit?
- “Yes, you need to follow-up with your family doctor in a week to check your blood pressure and to make sure that Tiazac®XC is working for you.”
- Do I need any tests and when do I book my next visit?
At the end of the dialogue, remind your loved one that it is also important to keep his/her medication record up-to-date. The record should include medications and changes made, and also the patient’s drug allergies, vitamins and minerals, herbals or natural health products, and any other non-prescription medications, such as over-the-counter medications. Keeping an up-to-date medication list is one way to keep track of changes and this also helps patients communicate the changes to healthcare providers in their circle of care.
Lastly, encourage patients to initiate a dialogue with their healthcare providers to assess for the possibility of reducing or stopping any of their medications in order to optimize their medication therapy management. If every patient can ask about his/her medications at hospital discharge, during visits to the doctor’s office and the community pharmacy, a significant number of medication incidents can be prevented.
Additional Resources:
- 5 Questions To Ask About Your Medications – https://www.ismp-canada.org/medrec/5questions.htm
- MyMedRec App – https://www.knowledgeisthebestmedicine.org/index.php/en/app/
Carol Nguyen completed a PharmD rotation at the Institute for Safe Medication Practices Canada (ISMP Canada) in 2016; Certina Ho is a Project Lead at ISMP Canada.