HN Summary
• Mackenzie Health is transforming hospital care for older adults, who make up 70% of its inpatients, by investing in specialized seniors-care training, dedicated expertise and a coordinated Seniors Care Strategy to improve safety, consistency and outcomes.
• Targeted initiatives such as the ADAPT delirium-prevention model, EMR-integrated screening tools and the specialized Behavioural Acute Care for the Elderly (BACE) Unit are helping staff prevent complications, deliver personalized care and support seniors with complex medical and cognitive needs.
• Looking ahead, Mackenzie Health’s refreshed Seniors Care Strategy (2025–2028) focuses on mobility, patient and family engagement, community partnerships and embedding senior-friendly practices into organization-wide training—building a future-ready system that supports seniors with dignity, compassion and evidence-based care.
At Mackenzie Health, seniors make up 70 per cent of inpatients, a reflection of Canada’s aging population and the complex health needs that come with it. Older adults often face multiple chronic conditions, cognitive challenges and heightened risks of hospital-acquired complications. Without a specialized approach, these vulnerabilities can lead to longer hospital stays, poorer outcomes and greater strain on patients, caregivers and the health system.
In response, Mackenzie Health is leading a transformation in seniors care, one grounded in compassion, evidence and a long-term commitment to helping seniors stay safe, engaged and supported.
Through specialized training, data-driven improvements and collaboration, Mackenzie Health is taking purposeful steps to enhance care for older adults. These efforts reflect its strategic focus on innovation, safety and continuous learning, an approach that’s helping build a more senior-friendly health system for the future.
“Transforming seniors care isn’t just a clinical priority; it’s a core responsibility we owe to those we care for,” says Heather Stewart, Interim Executive Vice President, Clinical Services and Chief Nursing Executive at Mackenzie Health. “Our goal is to create a system where every senior receives care that’s compassionate, consistent and tailored to their unique circumstances.”
Investing in expertise and education
This transformation began in 2023 with the creation of a dedicated seniors care specialist role to advance best practices in gerontology across the organization. From there, Mackenzie Health launched an organization-wide education campaign to equip nurses with the knowledge and tools to provide senior-friendly care every day.
The program offered two learning pathways: a six-hour foundational course, or a more in-depth “Senior Care Champion” program, both designed to develop nurses as role models and resources for their teams. The response was overwhelmingly positive: over one-third of nurses have completed specialized training, and 129 have become Senior Care Champions. This brings Mackenzie Health closer to its goal of having 30 per cent of staff on each unit serve in Champion roles, helping to embed a senior-friendly culture across the organization.
“We wanted every nurse to feel confident supporting seniors, not just in theory, but in real, practical ways,” says Peggy Richards, Clinical Nurse Specialist, Seniors Care. “That confidence translates directly into safer, more compassionate care.”
From education to system-wide improvement
Building on this early success, Mackenzie Health introduced its first Seniors Care Strategy in 2024 — a co-ordinated, evidence-based plan to ensure consistent, personalized and quality care for older adults. The strategy focuses on safety, resilience and continuous learning, principles that underpin Mackenzie Health’s broader commitment to high reliability and patient care excellence.
One of the strategy’s first priorities: preventing hospital acquired delirium.
Delirium is a sudden state of confusion or disorientation and is the third most common harmful event in hospitals and a major risk for seniors. Up to 64 per cent of hospitalized seniors are at risk of developing delirium, which can lead to longer stays, increased falls and cognitive decline.
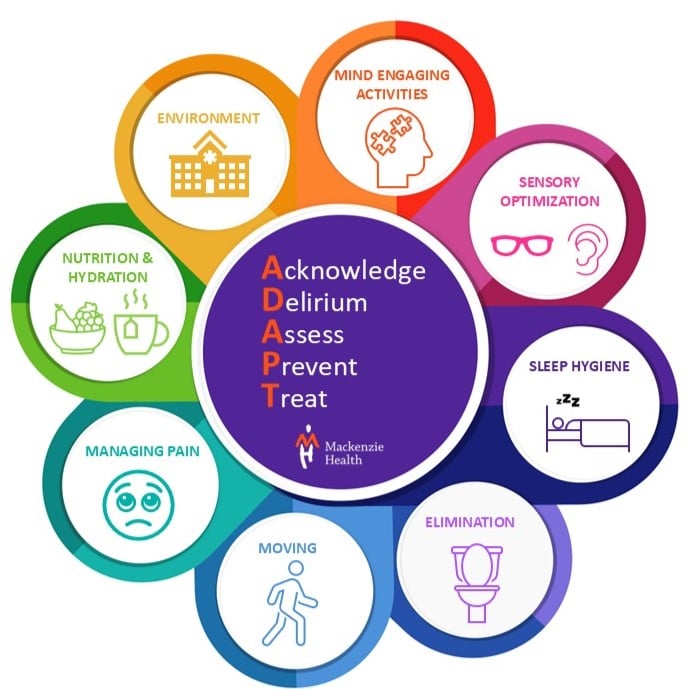
To address this, Mackenzie Health developed the ADAPT Model for delirium prevention, a practical framework that helps nurses recognize and reduce risk factors early:
• Acknowledge
• Delirium
• Assess every shift
• Prevent where possible
• Treat if it develops
The ADAPT model encourages staff to focus on eight key areas, from promoting mobility and good sleep to ensuring proper nutrition, hydration and sensory engagement.
“By addressing these areas every day, we’re helping patients stay alert, active and engaged, and that has a measurable impact on recovery,” says Richards.
To make this work seamless, Mackenzie Health integrated a delirium checklist into its electronic medical record (EMR) system. The tool tracks sreenings, flags positive results and supports documentation – ensuring every patient receives timely, co-ordinated care.
A specialized approach for complex needs
Mackenzie Health’s commitment extends beyond education and strategy to the design of its care spaces. In early 2023, it opened the Behavioural Acute Care for the Elderly (BACE) Unit, designed for patients with both acute medical needs and cognitive challenges such as delirium or dementia.
The 12-bed unit combines medical and behavioural expertise in a calming, senior-friendly environment. Bright lighting, floral murals and thoughtfully designed spaces help reduce confusion and agitation, while a specialized interprofessional team, including a psycho-geriatrician, nurse practitioner and behavioural specialist, provides integrated, holistic care.
“The BACE Unit shows what’s possible when we bring together design, expertise and compassion,” says Stewart. “It’s helping patients recover faster and with greater comfort.”
Looking ahead: evolving care for an aging community
With one in four York Region residents projected to be 65 or older by 2051, Mackenzie Health is ensuring its approach continues to evolve. The organization’s refreshed Seniors Care Strategy (2025–2028) builds on staff feedback and patient experiences to deliver tangible, system-wide improvements.
Key initiatives include developing a new mobility program to prevent falls and support safe movement during hospitalization, co-developing a seniors care toolkit with patients and families to enhance their education and engagement, and working to standardize clinical referral processes and strengthen community partnerships to ensure continuity of care beyond hospital walls.
To reinforce this work, Mackenzie Health will also integrate senior-friendly principles into its onboarding and annual training programs and provide foundational education on senior-friendly practices for staff across all roles, not just clinical teams.
These efforts reflect a proactive, holistic strategy to reduce preventable harm, improve patient outcomes and build a culture where senior-friendly care is a shared responsibility.
“We’re not just responding to demographic change, we’re preparing for the future,” says Stewart. “By investing in senior-friendly care today, we’re building a health system that grows with our community and sets new standards for excellence.”
From specialized training to technology-enabled care, Mackenzie Health’s work reflects a long-term commitment: ensuring every senior is cared for with safety, dignity and compassion.

