By Steffanie Strathdee
I never imagined that bacteria I used to streak on my petri plates back in the 1980’s at the University of Toronto would evolve to become ‘superbugs’ that have become increasingly resistant to antibiotics. As an infectious disease epidemiologist and a professor with academic appointments in both the US and Canada, I am ashamed to say that I was blindsided by the gravity of the global antimicrobial resistance (AMR) crisis until November 2015, when a family illness made this issue very personal.
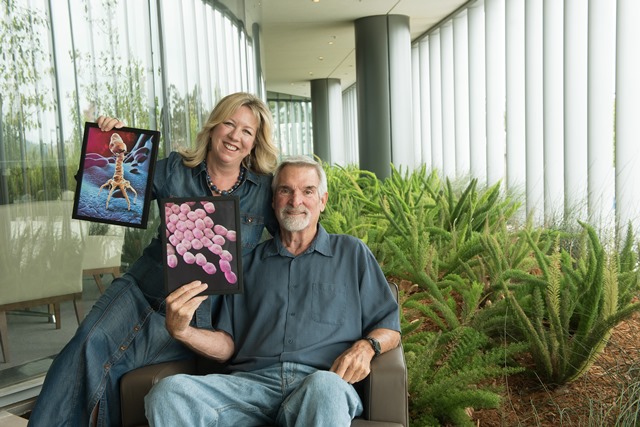
During a holiday to Egypt, my husband Tom suffered a gallstone attack and a superbug moved into the giant abscess that had formed inside his abdomen. It wasn’t a garden variety bacterium, but Acinetobacter baumannii, the World Health Organization’s #1 most dangerous superbug. Since I’d last met A.baumannii as an undergraduate in my virology class, it had evolved into a bacterial kleptomaniac that collected a treasure trove of antibiotic-resistance genes from other bacteria. By the time Tom was medevacked back to our home to San Diego, his bacterial isolate had become resistant to all antibiotics, even colistin and meropenem. Despite receiving top medical care, my husband was dying.
When I realized that Tom was about to become one of the estimated 1.5 million people who die from superbug infections every year I took matters into my own hands. Although I was not an MD, I knew how to conduct a literature review. I turned to PubMed, a publicly available database made available by the National Library of Medicine. Buried in the scientific literature was something that rang a bell from my U of T days: phage therapy.
Bacteriophages (phages for short) are the natural predators of bacteria. They were discovered in 1917 by Felix d’Herelle, a self-taught French-Canadian microbiologist. After dosing himself, his family and staff with a purified suspension of bacteriophages with no ill effects, d’Herelle used phages to treat a boy suffering from dysentery during an outbreak in Paris in 1919; the child was miraculously cured within 24 hours and subsequently, so were many others.
Phage therapy had a heyday in the 1920’s and 30’s, especially in the former Soviet Union, where d’Herelle helped a bacteriologist named Giorgi Eliava launch the first phage therapy center in what is now Tbilisi, Georgia. Meanwhile, in the West, phage therapy came under fire after several attempts at commercialization because some companies over-promised and under-delivered. No one knew at the time that phages needed to be matched to the specific bacteria they infected, and if they aren’t kept refrigerated they can be rendered useless. After penicillin was introduced in 1942, phage therapy was largely forgotten in the West. Since d’Herelle was considered an egotist with a tendency to infuriate his peers and anything resembling Russian was shunned during WWII, phage therapy was essentially abandoned for decades outside of the Republic of Georgia and Poland.
Antibiotics were one of the most important medical advances of the 20th Century but their use and mis-use, especially in livestock, meant that by the turn of the century, AMR was spreading faster than anyone imagined. In November 2015, the same month Tom fell ill, the mcr-1 gene that confers resistance to colistin, considered an antibiotic of last resort, was discovered in China, where it had been routinely given to pigs as a growth promotor . By the time the report was published in The Lancet, mcr-1 had spread to thirty countries. Tom’s bacterial isolate had it, along with 50 other AMR genes.
When I proposed treating Tom with phage therapy in early 2016, most of his physicians had never heard of it and almost all were skeptical. It was considered experimental by the Food and Drug Administration. But faced with a dying man who had no antibiotic options left, I am grateful that they were willing to give it a chance, provided I could find phages that matched his bacterial isolate.
With the help of PubMed, I managed to find phage researchers –a global village of total strangers – from the US, Belgium, Switzerland, India and even the US Navy Medical Research Center – who offered to undergo a phage hunt to see if they could find some to match Tom’s bacterial strain. Phage researchers from Texas A&M University (TAMU) turned their lab into the command centre. They tested not only characterized phages from established libraries but environmental samples from sewage, the ship bilges, barnyard waste and garbage dumps, since phage are best sourced from locations where there are vast quantities of bacteria.

Right after Tom’s case was presented at the Pasteur Institute’s 100th Anniversary of the discovery of bacteriophages in Paris in April, 2017 and again following publication of his case report, his doctors and I began receiving requests from all over the world from family members asking for phage therapy to save their loved ones from superbug infections. We were able to help some. Others sought treatment from Georgia, Poland or a new phage therapy center in Belgium. Some died before phages could reach them. In response to the growing number of requests, my colleagues and I founded the non-profit Center for Innovative Phage Applications and Therapeutics (IPATH) at UC San Diego (UCSD) in 2018. In 2019, the US National Institute of Health funded its first phage therapy trial in conjunction with the Antibiotic Resistance Leadership Group, and we will enroll our first patients in San Diego in 2020. Beyond moving phage therapy into clinical trials, we are also fundraising to develop a phage library to allow us to more quickly match phage to clinical isolates. In the meantime, we continue to assist with emergency requests for patients with superbug infections that are no longer responding to antibiotics. To date, IPATH has treated nine patients at UCSD, and dozens others in the US and internationally. We receive frequent requests from Canada and are working with a number of Canadian infectious disease physicians to develop protocols so that Health Canada can consider approval of compassionate use cases.
The pharmaceutical industry has been circumspect about phage therapy until relatively recently. However, the first successful use of genetically modified phage to treat a case of disseminated Mycobacterium abscessus in a teenager with cystic fibrosis in the UK has piqued their interest, since genetically altered phage are easier to patent. Further, since phage-antibiotic combinations can be synergistic, phage can also be used indirectly to re-sensitize bacteria to antibiotics they were resistant to. More research is needed to enable clinicians to rapidly identify and exploit these relationships. Looking ahead, the advent of synthetic phage cocktails is likely to expand treatment options even further.
While it is unlikely that phage therapy will ever replace antibiotics, it is a promising alternative and/or adjunct therapy that deserves to be rigorously evaluated in clinical trials. Given that the global AMR crisis is worsening and is considered to be a more immediate threat to human health than climate change, we cannot afford to allow a promising alternative to be forgotten for another hundred years.
Steffanie Strathdee, PhD is the Associate Dean of Global Health Sciences, Harold Simon Professor, University of California San Diego Department of Medicine Co-Director, Center for Innovative Phage Applications and Therapeutics and author of The Perfect Predator: A Scientist’s Race to Save her Husband from a Deadly Superbug For more information visit: ThePerfectPredator.com