By Sheryl Gray
Addiction doesn’t discriminate, so why should we?
Addiction affects all walks of life…people with families, jobs, disabilities…it’s not always possible for people to enter into a residential treatment program away from home. For some, accessibility is an issue. For others, the associated stigma of “going to detox” keeps them from seeking help.
Detox isn’t a place, it’s a process.
The START program is a new two-week, in-home detox program for Vancouver residents, aimed at people who need help to stop or stabilize their substance use. The program is completed at home, with no wait required: Clients can begin their detox journey within 24 hours of referral.
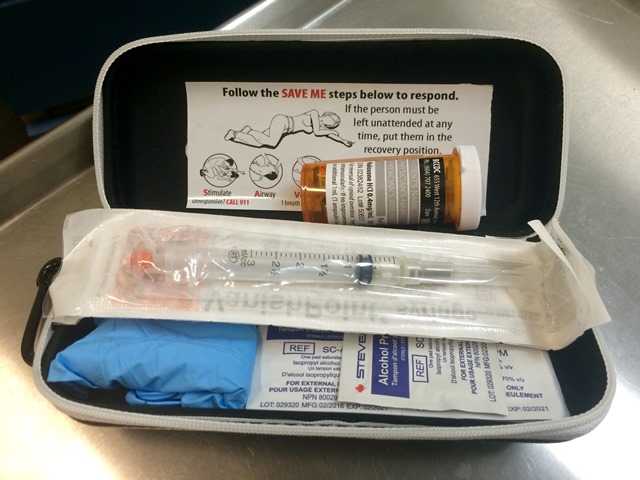
The START team provides same-day or next-day intake for new referrals (professional or self-made). The first step is a visit to the program’s office, at a local Community Health Centre. Each client receives a thorough assessment by a nurse and doctor, and also has a home assessment completed to ensure a stable and supported environment is available. For the first five days of the program, a START nurse visits twice daily to monitor the detox process. During the second week, connections are made to other resources that will be essential to the client’s unique recovery process.
“Medication-based treatment alone is not holistic care for addictions. Psychosocial, emotional and spiritual care are at least as important as the medical care,” says Dr. John Álvarez de Lorenzana, physician with the START program. “Clients who come to START will encounter service providers who are trained in a trauma-informed approach, and receive supported, compassionate care. We have the fortunate advantage of being part of the larger Vancouver Coastal Health network, with direct access to many medical and mental health care programs.”

Dr. Álvarez de Lorenzana believes that addiction is becoming more accepted and understood as a chronic disease, a piece of treatment that’s been absent in the past. Medications, such as Suboxone —which is considered a safer opioid replacement than methadone — play an important role in harm reduction and engagement in recovery activities and daily functioning. This helps people stabilize over time, which allows them to turn their focus to healing the other areas of their life from where the addiction stems. The initial medical detox process is really just the beginning of the journey, and provides a foundation for the hard work which must follow for recovery.
Sheryl Gray is a Communications Specialist at Vancouver Coastal Health.




